1: EMDR Therapy Overview
The world is round and the place which may seem like the end may also be the beginning.
—Ivy Baker Priest (Parade, 1958)
REINTRODUCTION TO EMDR THERAPY
The goal of
(Shapiro, 2018, p. 6)
This chapter summarizes the information covered in the most recent
Although the
Extensive familiarity with Dr. Shapiro’s primary text is a prerequisite for the reading of this Primer, which is intended to supplement, not replace, her required pre-training readings. No clinician who intends to utilize
There have been other offshoots of
TRAUMA
WHAT IS TRAUMA?
The diagnostic criteria for posttraumatic stress disorder (
the state of severe fright that we experience when we are confronted with a sudden, unexpected, potentially life-threatening event, over which we have no control, and to which we are unable to respond effectively no matter how hard we try (1995).
A child who was sexually abused by her older brother may grow up to believe “I am bad” or “The world is unsafe.” When an individual experiences a traumatic event, the event can become entrenched (or fixed) in the form of irrational beliefs, negative emotions, blocked energy, and/or physical symptoms, such as anxieties, phobias, flashbacks, nightmares, and/or fears. Regardless of the magnitude of the trauma, it may have the potential for negatively impacting an individual’s self-confidence and self-efficacy. The event can become locked or “stuck” in the memory network (i.e., “an associated system of information” [Shapiro, 2018, p. 30]) in its original form, causing an array of traumatic or
TYPES OF TRAUMA
Dr. Shapiro (2018) distinguishes between big “T” traumas and other adverse life experiences or disturbing life events (formerly referred to as small “t” traumas). When a person hears the word “trauma,” experiences and images of man-made events such as fires, explosions, automobile accidents, or natural disasters, which include hurricanes, floods, and tornadoes, emerge. Sexual abuse, a massive heart attack, death of a loved one, Hurricane Katrina, and the 9/11 attacks on the World Trade Center by international terrorists are graphic examples of big “T” traumas. Among other descriptors, these types of traumas can be defined as dangerous and life threatening and fit the criteria in the
Then there are the traumas Shapiro (2018) has designated as adverse life experiences. These types of events may be subtler and tend to impact one’s beliefs about self, others, and the world. Adverse life experiences are those that can affect our sense of self, self-esteem, self-definition, self-confidence, and optimal behavior. They influence how we see ourselves as a part of the bigger whole. They are often ubiquitous (i.e., constantly encountered) in nature and are stored in state-dependent mode in our memory network. Unless persistent throughout the client’s childhood, adverse life experiences usually do not have much impact on overall development, yet maintain the ability to elicit negative self-attributions and have potential for other long-term negative consequences. The clinical presentations that often signal the presence of past adverse life events may be low self-esteem and anxiety as well as panic disorders and/or phobias, depression, posttraumatic symptoms, and the presence of dissociative disorders. The domains of dysfunction tend to be emotional, somatic, cognitive, and relational.
To illustrate the difference between an adverse life experience and a big “T” trauma, let us consider the case of Rebecca, who grew up as “the minister’s daughter.” As the offspring of a local pastor, Rebecca grew up, figuratively speaking, in a glass house. She believed that her father’s job rested on her behavior inside and outside of her home. In her world, everyone was watching. She was always in the spotlight, and no one seemed to want to share his or her life with her. She went through childhood with few friends. “I remember before and after church, the groups of kids forming. I was the outsider. No one invited me in.” All the kids were afraid that every move they made would be reported to her daddy. Being at home was not much better. Her father was never home. He was always out “tending to his flock” and had little time left for his own family. Her mother was not of much comfort either, because she spent much of her time trying to be perfect as well. Living in a glass house was not easy for any of them, especially Rebecca, the oldest of three. By the time Rebecca entered therapy, she was a wife and mother. She thought she had to be perfect in motherhood and in her marriage as well. She became frustrated, angry, and lonely. She felt misunderstood and neglected by her husband. He was never there. He never listened. She thought she could do nothing right, as hard as she tried.
Probing into Rebecca’s earliest childhood memories, no tragic or traumatic memories (i.e., big “T” traumas) emerged. As she continued to explore her past, the hardships and rigors of living in a glass house as the preacher’s daughter slowly became apparent. The original target that initiated a round of
The differentiation between adverse life experiences and big “T” traumas often appears too simplistic. Another way of discussing the types of trauma is to look at it in terms of shock or developmental trauma.
Shock trauma involves a sudden threat that is perceived by the central nervous system as overwhelming and/or life threatening. It is a single-episode traumatic event. Examples include car accidents, violence, surgery, hurricanes and other natural disasters, rape, battlefield assaults, and war.
Developmental trauma refers to events that occur over time and gradually affect and alter a client’s neurological system to the point that it remains in a traumatic state. This type of trauma may cause interruptions in a child’s natural psychological growth. Examples of developmental trauma are abandonment or long-term separation from a parent, an unstable or unsafe environment, neglect, serious illness, physical or sexual abuse, and betrayal at the hands of a caregiver. This type of trauma can have a negative impact on a child’s sense of safety and security in the world and tends to set the stage for future trauma in adulthood as the sense of fear and helplessness that accompany it goes unresolved.
Table 1.1 outlines more definitely the differences between big “T” traumas and adverse life experiences or disturbing life events (i.e., small “t” traumas).
ADAPTIVE INFORMATION PROCESSING—“THE PAST DRIVES THE PRESENT”
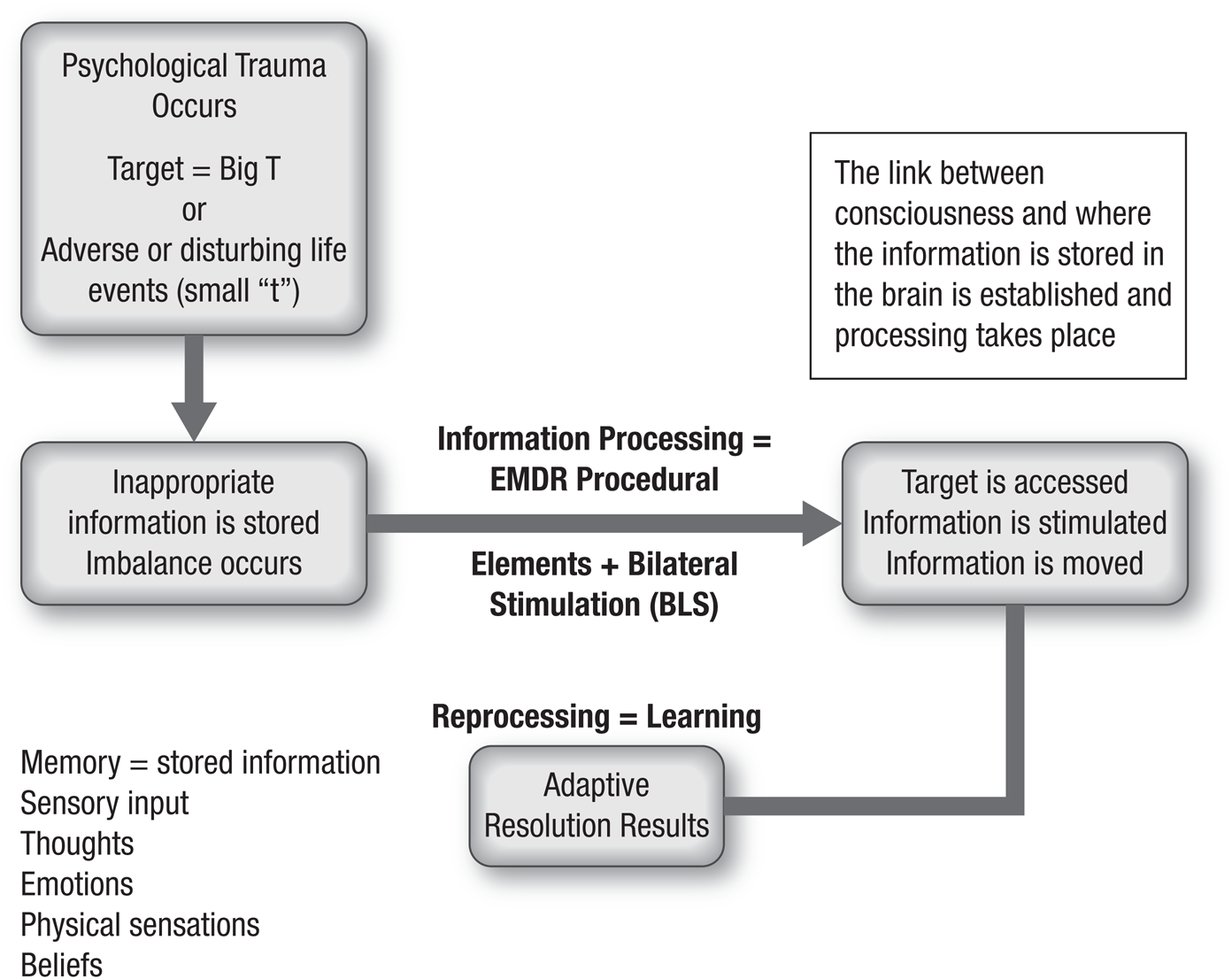
Dr. Francine Shapiro developed a hypothetical information processing model of learning called the
| BIG “T” TRAUMA | SMALL “t” TRAUMA (DISTURBING/DISTRESSING LIFE EVENTS) |
|---|---|
| Major event normally seen as traumatic May be a single- or multiple-event trauma May be pervasive Most often there is intrusive imagery Still elicits similar negative beliefs, emotions, and physical sensations Lasting negative effect on the client’s sense of safety in the world | Disturbing/distressing life event that may not always be perceived as traumatic More common and ubiquitous; usually accumulates over time from childhood More often it is pervasive and ongoing Often there is no intrusive imagery Still elicits similar negative beliefs, emotions, and physical sensations Lasting negative effect on the client’s sense of self (self-confidence, self-esteem, self-definition) |
| Examples: Serious accidents (e.g., automobile or bike accidents, plane crashes, serious falls) Natural disasters (e.g., earthquakes, tornadoes, tsunamis, forest fires, volcanic eruptions, floods) Man-made disasters (e.g., 9/11, explosions, fires, wars, acts of terrorism) Major life changes (e.g., serious illnesses, loss of loved ones) Physical and sexual assaults Major surgeries, life-threatening illnesses (e.g., cancer, heart attacks, craniotomies, heart bypasses) Ongoing life events (e.g., sexual abuse, domestic violence) War- and combat-related incidents | Examples: Moving multiple times during childhood Excessive teasing or bullying Persistent physical illnesses Constant criticism Rejections Betrayals Disparaging remarks Losing jobs Divorce or witnessing parental conflict Unmet developmental needs Death of pets Public shaming, humiliation, or failure Unresolved guilt Physical or emotional neglect Getting lost Chronic harassment |
| ACCELERATED INFORMATION PROCESSING (HOW IT IS USED) | |
|---|---|
| Working hypothesis | Working model |
| Explains how | Explains why |
| Developed to explain the rapid manner in which clinical results are achieved | Developed to explain the clinical phenomena observed |
| Simple desensitization treatment effect | Entails an information processing effect |
Abbreviation:

Shapiro (2018) posits that inherent in the
On the other hand, when a trauma occurs that is too large for your system to adequately process, it can become “stuck” (i.e., dysfunctionally stored) in the central nervous system. Maladaptive responses, such as flashbacks or dreams, can be triggered by present stimuli, and there may be attempts of the information processing system to resolve the trauma (Shapiro, 2018). When the system becomes overloaded as just described,
| ADAPTIVE | MALADAPTIVE |
|---|---|
| Big “T” (e.g., safety) | |
| I survived. I can learn from this. I can protect myself. I am safe. | Driving phobia Flashbacks Intense driving anxiety Night terrors |
| Small “t” (i.e., adverse or disturbing/distressing life events; e.g., responsibility) | |
| I am fine as I am. I did the best I could. I am significant/important. | Low self-esteem Irrational guilt Self-neglect, co-dependence |
| TARGET | |
|---|---|
| When the target is a disturbing memory. | When the target is positive (i.e., an alternative desirable imagined future). |
| Negative images, beliefs, and emotions become less vivid, less enhanced, and less valid. | Positive images, beliefs, and emotions become more vivid, more enhanced, and more valid. |
| Before reprocessing, links to dysfunctional material. | Links with more appropriate information. |
| Learning is a continuum. |
The
At the time of disturbing or traumatic events, information may be stored in the central nervous system in state-specific form (i.e., the negative cognitive belief and emotional and physical sensations the client experienced at the time of the traumatic event remain stored in the central nervous system just as if the trauma is happening in the now). Over time, a client may develop repeated negative patterns of feeling, sensing, thinking, believing, and behaving as a result of the dysfunctionally stored material. These patterns are stimulated, activated, or triggered by stimuli in the present that cause a client to react in the same or similar ways as in the past. Shapiro (2018) states throughout her basic text that the negative beliefs and affect from past events spill into the present. By processing earlier traumatic memories,
Abbreviation:
| DYSFUNCTIONALLY STORED MEMORIES | ADAPTIVELY STORED MEMORIES |
|---|---|
| Information processing system is overwhelmed and becomes “stuck” Embraces an inappropriate, developmentally arrested lack of power in the past | Information processing system is able to connect to current information and resources and adequately process information Embraces an age-appropriate power in the present |
| Past-oriented or developmentally arrested, dysfunctional perspective Stored in incorrect form of memory (i.e., implicit/motoric) Past is present | Present-oriented and age-appropriate, adaptive perspective Stored in correct form of memory (i.e., explicit/narrative) Past is past |
| ACCESS Frozen dysfunctional memory |
| STIMULATE Information processing system |
| MOVE Information to adaptive resolution |
| RESULTS Lessening of disturbance Gained information and insights Changes in emotional and physical responses |
Cognitive behavioral techniques, such as systematic desensitization, imaginal exposure, or flooding, require the client to focus on anxiety-provoking behaviors and irrational thoughts or to relive the trauma or other adverse life experiences.
Changes in perception and attitude, experiencing moments of insight, and subtle differences in the way a person thinks, feels, behaves, and believes are byproducts as well. The changes can be immediate. Take, for instance, a session with a young woman who had been brutally raped by her ex-boyfriend. During the Assessment Phase, Andrea’s terror appeared raggedly etched in her face and slumped demeanor. After many successive sets of bilateral stimulation (

Exhibit 1.2 demonstrates in action the inherent information processing mechanism as it highlights the changes that occurred as a result of Andrea and Billy’s dynamic drive toward mental health with
Because the heart of
| BEFORE | AFTER | |
|---|---|---|
| Client experiences negative event, resulting in: Intrusive images Negative thoughts or beliefs Negative emotions and associated physical sensations | Negative experience is transmuted into an adaptive learning experience | Client experiences adaptive learning, resulting in: No intrusive images No negative thoughts or beliefs No negative emotional and/or physical sensations An empowering new positive self-belief |
| What happens? Information is insufficiently (dysfunctionally) stored Dysfunctional information gets replayed Developmental windows may be closed | What happens? Information is sufficiently (adaptively) processed Adequate learning has taken place Development continues on a normal trajectory | |
| Resulting in: Depression Anxiety Low self-esteem Self-deprecation Powerlessness Inadequacy Lack of choice Lack of control Dissociation | Resulting in: Sense of well-being Self-efficacy Understanding Catalyzed learning Appropriate changes in behavior Emergence of adult perspective Self-acceptance Ability to be present |
Abbreviation:
Using an example of a traumatic event, 1.8 illustrates more graphically what happens during reprocessing of a traumatic event.
For a more comprehensive explanation of
As the previous tables and figures demonstrate,
MODEL, METHODOLOGY, AND MECHANISM OF EMDR THERAPY
Why and how does
| NEGATIVE EXPERIENCE | ADAPTIVE LEARNING EXPERIENCE | |
|---|---|---|
| Example: After a heated argument, Mary is raped by her ex-boyfriend in the parking lot of a bar they just left. | ||
| Mary experiences: Intrusive images: Negative thoughts and self-beliefs (e.g., I am a bad person) Negative emotions (e.g., shame, fear, anger, anxiety) Negative physical sensations (e.g., heart palpitations, sweaty palms, difficulty breathing) Sense of powerlessness Lack of choice Lack of control Inadequacy | Learning is catalyzed | Mary experiences: Cognitive restructuring of perceptions Association to positive affects Sense of well-being and self-efficacy New insights Feelings of empowerment Learning Greater sense of understanding |
Model—The
AIP model provides the theoretical model forEMDR therapy.Methodology—Eight phases of
EMDR therapy plus the ethics, safeguards, and validated modifications for basic and specific clinical situations and populations.Mechanism—Current hypotheses on how and why
EMDR therapy works on a neurobiological level.
MODEL—HOW?
The
Guided by this information processing model, memory networks are believed to form the basis of clinical symptoms and mental health in general, and “unprocessed memories are considered to be the primary basis of pathology” (Shapiro, 2009–2017a). The important components of the model as outlined by Shapiro (1995, 2001, 2018, 2009–2017a, 2009–2017b) are summarized in Table 1.9.
There is a body of literature, including both research and case reports on a variety of clinical complaints, that illustrates the predictive value of the
| The |
| Disturbing memories are dysfunctionally stored (i.e., perceived in the same way as when the memory was originally formed) and may disrupt the information processing system. |
| Emotions, physical sensations, and thoughts and beliefs associated with unprocessed memories are experienced by the client as their perceptions in the present link to the historical memory networks. |
| In order to be interpreted, a client’s perceptions of resent situations link into networks of physically stored memories (negative or dysfunctional) from the past. In other words, the past is present. |
| As the processing begins, disruptions may be caused by high levels of emotional disturbance or dissociation, which can block adaptive processing. |
| When a client is processing the memory of a traumatic event, they have the opportunity to forge adaptive associations with memory networks of functional information stored in the brain. This |
| During processing, the unprocessed elements of a client’s memory (i.e., image, thoughts, sounds, emotional and physical sensations, beliefs) have the ability to transform/transmute to an adaptive resolution. At this point, learning may take place. By discarding maladaptive information and storing adaptive information, a client has new learning that may better inform future experiences and choices. |
Abbreviation:
METHODOLOGY—HOW/WHAT?
For further reading on the “how” and “what” of
| 1997 Brown, K. W., McGoldrick, T., & Buchanan, R. (1997). Body dysmorphic disorder: Seven cases treated with eye movement desensitization and reprocessing. Behavioural and Cognitive Psychotherapy, 25(2), 203–207. https://doi.org/10.1017/S1352465800018403 |
| 1998 Felitti, V. J., Anda, R. F., Nordenberg, D., Williamson, D. F., Spitz, A. M., Edwards, V., Koss, M. P., & Marks, J. S. (1998). Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The adverse childhood experiences ( |
| 2001 Ray, A. L., & Zbik, A. (2001). Cognitive behavioral therapies and beyond. In C. D. Tollison, J. R. Satterhwaite, & J. W. Tollison (Eds.). Practical pain management (3rd ed., pp. 189–208). Lippincott. Shapiro, F. (2001). Eye movement desensitization and reprocessing: Basic principles, protocols, and procedures (2nd ed.). Guilford Press. |
| 2002 Perkins, B., & Rouanzoin, C. (2002). A critical evaluation of current views regarding eye movement desensitization and reprocessing ( Shapiro, F. (2002). |
| 2004 Heim, C., Plotsky, P. M., & Nemeroff, C. B. (2004). Importance of studying the contributions of early adverse experience to neurobiological findings in depression. Neuropsychopharmacology, 29, 641–648. https://doi.org/10.1038/sj.npp.1300397 |
| 2005 Gold, S. D., Marx, B. P., Soler-Baillo, J. M., & Sloan, D. M. (2005). Is life stress more traumatic than traumatic stress? Journal of Anxiety Disorders, 19, 687–698. https://doi.org/10.1016/j.janxdis.2004.06.002 Mol, S. S. L., Arntz, A, Metsemakers, J. F. M, Dinant, G., Vilters-Van Montfort, P. A. P., & Knottnerus, A. (2005). Symptoms of post-traumatic stress disorder after non-traumatic events: Evidence from an open population study. British Journal of Psychiatry, 186, 494–499. https://doi.org/10.1192/bjp.186.6.494 |
| 2006 Brown, S., & Shapiro, F. (2006). Madrid, A., Skolek, S., & Shapiro, F. (2006). Repairing failures in bonding through Raboni, M. R., Tufik, S., & Suchecki, D. (2006). Treatment of Ricci, R. J., Clayton, C. A., & Shapiro, F. (2006). Some effects of Shapiro, F. (2006). New notes on adaptive information processing: Case formulation principles, scripts, and worksheets. Uribe, M. E. R., & Ramirez, E. O. L. (2006). The effect of Wilensky, M. (2006). Eye movement desensitization and reprocessing ( |
| 2007 Fernandez, I., & Faretta, E. (2007). Eye movement desensitization and reprocessing in the treatment of panic disorder with agoraphobia. Clinical Case Studies, 6(1), 44–63. https://doi.org/10.1177/1534650105277220 Schneider, J., Hofmann, A., Rost, C., & Shapiro, F. (2007). Shapiro, F. (2007a). Shapiro, F. (2007b). Shapiro, F., Kaslow, F. W., & Maxfield, M. (2007). Handbook of |
| 2008 Bae, H., Kim, D., & Park, Y. C. (2008). Eye movement desensitization and reprocessing for adolescent depression. Psychiatry Investigation, 5(1), 60–65. https://doi.org/10.4306/pi.2008.5.1.60 Gauvreau, P., & Bouchard, S. (2008). Preliminary evidence for the efficacy of McGoldrick, T., Begum, M., & Brown, K. W. (2008). |
| 2008 Russell, M. C. (2008). Treating traumatic amputation-related phantom limb pain: A case study utilizing eye movement desensitization and reprocessing within the Armed Services. Clinical Case Studies, 7(2), 136–153. https://doi.org/10.1177/1534650107306292 Schneider, J., Hofmann, A., Rost, C., & Shapiro, F. (2008). Solomon, R. M., & Shapiro, F. (2008). |
| 2009 Wesselmann, D., & Potter, A. E. (2009). Change in adult attachment status following treatment with |
| 2010 de Roos, C., Veenstra, A., de Jongh, A., den Hollander-Gijsman, M., van der Wee, N., Zitman, F., & van Rood, Y. R. (2010). Treatment of chronic phantom limb pain using a trauma-focused psychological approach. Pain Research & Management, 15(2), 65–71. https://doi.org/10.1155/2010/981634 Obradovic, J., Bush, N. R., Stamperdahl, J., Adler, N. E., & Boyce, W. T. (2010). Biological sensitivity to context: The interactive effects of stress reactivity and family adversity on socioemotional behavior and school readiness. Child Development, 1, 270–289. https://doi.org/10.1111/j.1467-8624.2009.01394.x Robinson, J. S., & Larson, C. (2010). Are traumatic events necessary to elicit symptoms of posttraumatic stress? Psychological Trauma: Theory, Research, Practice, and Policy, 2, 71–76. https://doi.org/10.1037/a0018954 Teicher, M. H., Samson, J. A., Sheu, Y.-S., Polcari, A., & McGreenery, C. E. (2010). Hurtful words: Association of exposure to peer verbal abuse with elevated psychiatric symptom scores and corpus callosum abnormalities. American Journal of Psychiatry, 167, 1464–1471. https://doi.org/10.1176/appi.ajp.2010.10010030 |
| 2011 Arseneault, L., Cannon, M., Fisher, H. L., Polanczyk, G., Moffitt, T. E., & Caspi, A. (2011). Childhood trauma and children’s emerging psychotic symptoms: A genetically sensitive longitudinal cohort study. American Journal of Psychiatry, 168, 65–72. https://doi.org/10.1176/appi.ajp.2010.10040567 Heins, M., Simons, C., Lataste, T., Pfeifer, S., Versmissen, D., Lardinois, M., Marcelis, M., Delespaul, P., Krabbendam, L., van Os, J., & Myin-Germeys, I. (2011). Childhood trauma and psychosis: A case-control and case-sibling comparison across different levels of genetic liability, psychopathology, and type of trauma. American Journal of Psychiatry, 168, 1286–1294. https://doi.org/10.1176/appi.ajp.2011.10101531 |
| 2011 Nazari, H., Momeni, N., Jariani, M., & Tarrahi, M. J. (2011). Comparison of eye movement desensitization and reprocessing with citalopram in treatment of obsessive-compulsive disorder. International Journal of Psychiatry in Clinical Practice, 15(4), 270–274. https://doi.org/10.3109/13651501.2011.590210 |
| 2012 Afifi, T. O., Mota, N. P., Dasiewicz, P., MacMillan, H. L., & Sareen, J. (2012). Physical punishment and mental disorders: Results from a nationally representative Shapiro, F. (2012a). van den Berg, D. P. G., & van der Gaag, M. (2012). Treating trauma in psychosis with Varese, F., Smeets, F., Drukker, M., Lieverse, R, Lataster, T., Viechtbauer, W., Read, J., van Os, J., & Bentall, R. P. (2012). Childhood adversities increase the risk of psychosis: A meta-analysis of patient-control, prospective-and cross-sectional cohort studies. Schizophrenia Bulletin, 38(4), 661–671. https://doi.org/10.1093/schbul/sbs050 |
| 2013 Doering, S., Ohlmeier, M.-C., de Jongh, A., Hofmann, A., & Bisping, V. (2013). Efficacy of a trauma-focused treatment approach for dental phobia: A randomized clinical trial. European Journal of Oral Sciences, 121(6), 584–593. https://doi.org/10.1111/eos.12090 Faretta, E. (2013). |
| 2014 Read, J., Fosse, R., Moskowitz, A., & Perry, B. (2014). The traumagenic neurodevelopmental model of psychosis revisited. Neuropsychiatry, 4(1), 65–79. https://doi.org/10.2217/NPY.13.89 Shapiro, F. (2014). The role of eye movement desensitization and reprocessing ( |
| 2015 Allon, M. (2015). Behnam Moghadam, M., Alamdari, A. K., Behnam Moghadam, A., & Darban, F. (2015). Effect of |
| 2018 Shapiro, F. (2018). Eye movement desensitization and reprocessing: Basic principles, protocols and procedure (3rd ed.). Guilford Press. Gauhar, M., & Wajid, Y. (2016). The efficacy of |
MECHANISM—WHY?
Over the past 25 years, numerous studies have indicated that eye movements have effects on a client’s memory in terms of vividness, retrieval, emotional arousal, and more. Studies that evaluated
| 1996 Andrade, J., Kavanagh, D., & Baddeley, A. (1997). Eye-movements and visual imagery: A working memory approach to the treatment of post-traumatic stress disorder. British Journal of Clinical Psychology, 36, 209–223. https://doi.org/10.1111/j.2044–8260.1997.tb01408.x Armstrong, M. S., & Vaughan, K. (1996). An orienting response model of eye movement desensitization. Journal of Behavior Therapy & Experimental Psychiatry, 27, 21–32. https://doi.org/10.1016/0005-7916(95)00056-9 MacCulloch, M. J., & Feldman, P. (1996). Eye movement desensitization treatment utilizes the positive visceral element of the investigatory reflex to inhibit the memories of post-traumatic stress disorder: A theoretical analysis. British Journal of Psychiatry, 169(5), 571–579. https://doi.org/10.1192/bjp.169.5.571 Wilson, D., Silver, S. M., Covi, W., & Foster, S. (1996). Eye movement desensitization and reprocessing: Effectiveness and autonomic correlates. Journal of Behaviour Therapy and Experimental Psychiatry, 27, 219–229. https://doi.org/10.1016/S0005-7916(96)00026-2 |
| 1999 Lipke, H. (1999). Comments on “thirty years of behavior therapy” and the promise of the application of scientific principles. The Behavior Therapist, 22, 11–14. Rogers, S., Silver, S., Goss, J., Obenchain, J., Willis, A., & Whitney, R. (1999). A single session, controlled group study of flooding and eye movement desensitization and reprocessing in treating posttraumatic stress disorder among Vietnam war veterans: Preliminary data. Journal of Anxiety Disorders, 13, 119–130. |
| 2000 Bergmann, U. (2000). Further thoughts on the neurobiology of |
| 2001 Kavanagh, D. J., Freese, S., Andrade, J., & May, J. (2001). Effects of visuospatial tasks on desensitization to emotive memories. British Journal of Clinical Psychology, 40, 267–280. https://doi.org/10.1348/014466501163689 |
| 2002 Rogers, S., & Silver, S. M. (2002). Is Stickgold, R. (2002). |
| 2004 Barrowcliff, A. L., Gray, N. S., Freeman, T. C. A., & MacCulloch, M. J. (2004). Eye movements reduce the vividness, emotional valence and electrodermal arousal associated with negative autobiographical memories. Journal of Forensic Psychiatry and Psychology, 15(2), 325–345. https://doi.org/10.1080/14789940410001673042 Suzuki, A., Josselyn, S. A., Frankland, P. W., Masushige, S., Silva, A. J., & Satoshi, K. (2004). Memory reconsolidation and extinction have distinct temporal and biochemical signatures. Journal of Neuroscience, 24(20), 4787–4795. https://doi.org/10.1523/jneurosci.5491-03.2004 |
| 2006 Lee, C. W., Taylor, G., & Drummond, P. D. (2006). The active ingredient in Servan-Schreiber, D., Schooler, J., Dew, M. A., Carter, C., & Bartone, P. (2006). |
| 2007 Propper, R., Pierce, J. P., Geisler, M. W., Christman, S. D., & Bellorado, N. (2007). Effect of bilateral eye movements on frontal interhemispheric gamma |
| 2008 Bergmann, U. (2008). The neurobiology of Sack, M., Hofmann, A., Wizelman, L., & Lempa, W. (2008). Psychophysiological changes during Sack, M., Lempa, W., Steinmetz, A., Lamprecht, F., & Hofmann, A. (2008). Alterations in autonomic tone during trauma exposure using eye movement desensitization and reprocessing ( Elofsson, U. O. E., von Scheele, B., Theorell, T., & Sondergaard, H. P. (2008). Physiological correlates of eye movement desensitization and reprocessing. Journal of Anxiety Disorders, 22, 622–634. https://doi.org/10.1016/j.janxdis.2007.05.012 |
| 2008 Stickgold, R. (2008). Sleep-dependent memory processing and |
| 2009 Friedman, D., Goldman, R., Stern, Y., & Brown, T. (2009). The brain’s orienting response: An event-related functional magnetic resonance imaging investigation. Human Brain Mapping, 30(4), 1144–1154. Gunter, R., & Bodnar, G. (2009). Lilley, S. A., Andrade, J., Turpin, G., Sabin-Farrell, R., & Holmes, E. A. (2009). Visuospatial working memory interference with recollections of trauma. British Journal of clinical psychology, 48(3), 309–321. |
| 2010 Bergmann, U. (2010). Hornsveld, H. K., Landwehr, F., Stein, W., Stomp, M., Smeets, S., & van den Hout, M. A. (2010). Emotionality of loss-related memories is reduced after recall plus eye movements but not after recall plus music or recall only. Journal of Kapoula, Z., Yang Q., Bonnet, A., Bourtoire, P., & Sandretto, J. (2010). van den Hout, M. A., Engelhard, I. M., Smeets, M. A., Hornsveld, H., Hoogeveen, E., & de Heer, E. (2010). Counting during recall: Taxing of working memory and reduced vividness and emotionality of negative memories. Applied Cognitive Psychology, 24(3), 303–311. https://doi.org/10.1002/acp.1677 |
| 2011 El Khoury-Malhame, M., Lanteaume, L., Beetz, E. M., Roques, J., Reynaud, E., Samuelian, J.-C., Blin, O., Garcia, R., & Khalfa, S. (2011). Attentional bias in post-traumatic stress disorder diminishes after symptom amelioration. Behavior Research and Therapy, 49(11), 796–801. https://doi.org/10.1016/j.brat.2011.08.006 Kristjánsdóttir, K., & Lee, C. M. (2011). A comparison of visual versus auditory concurrent tasks on reducing the distress and vividness of aversive autobiographical memories. Journal of |
| 2012 van den Hout, M., & Engelhard, I. (2012). How does van den Hout, M. A., Rijkeboer, M. M., Engelhard, I. M., Klugkist, I., Hornsveld, H., Toffolo, M. J., & Cath, D. C. (2012). Tones inferior to eye movements in the |
| 2013 de Jongh, A., Ernst, R., Marques, L., & Hornsveld, H. (2013). The impact of eye movements and tones on disturbing memories involving Pagani, M., Hogberg, G., Fernandez, I., & Siracusano, A. (2013). Correlates of |
| 2014 Leer, Engelhard, and van den Hout provided corroborating evidence that recall with |
| 2016 van Schie, K., Engelhard, I. M., Klugkist, I., & van den Hout, M. A. (2016). Blurring emotional memories using eye movements: Individual differences and speed of eye movements. European Journal of Psychotraumatology, 7, 29476. https://doi.org/10.3402/ejpt.v7.29476 van Veen, S. C., Engelhard, I. M., & van den Hout, M. A. (2016). The effects of eye movements on emotional memories: Using an objective measure of cognitive load. European Journal of Psychotraumatology, 7, 30122. https://doi.org/10.3402/ejpt.v7.30122 |
| 2018 Calancie, O. G., Khalid-Khan, S., Booij, L., & Munoz, D. P. (2018). Eye movement desensitization and reprocessing as a treatment for |
Abbreviation:
THREE-PRONGED APPROACH
PAST, PRESENT, FUTURE
Regardless of what you as a participant were taught in the earlier didactic trainings, what you most likely will remember is what was on the instructional sheet that sat on your lap. The first question that you asked the client was, “What old issue or old memory would you like to focus on today?” It is important to note that this question was only used in the training exercises and not in daily clinical practice. Fortunately, this teaching method has changed as the training focus now is to establish a more formalized plan that attempts to identify past events (and a touchstone event, if available), present triggers, and a future template, and to encourage the participant to process in this order. Shapiro (2006) referred to this strategy as the Treatment Planning Guide (

To completely resolve a client’s issue and achieve adaptive resolution,
THREE-PRONGED TARGETS—EXPERIENTIAL CONTRIBUTORS TO PRESENT-DAY PROBLEMS
The order of the processing is important. First, it is necessary to strive to adaptively resolve past traumas, then process current stimuli that trigger distress, and finally do a future template on the present trigger. See Exhibit 1.3 for a breakdown of what is identified and processed under each prong of the
The clinician may want to consider targeting the memories that lay the groundwork for any present problems and/or issues first. It may be a single traumatic event or what is called a touchstone event, a primary and self-defining event in the client’s life. In
Once all presently charged past events are processed (i.e., after the touchstone event is processed), other past events may or may not have a cognitive or affective charge remaining. The clinician may want to consider processing those that have a “charge” before continuing to recent events. Then any recent events, circumstances, situations, stressors, or other triggers that might elicit a disturbance are targeted. After the past events and present disturbances have been identified and reprocessed, focus on the future desired behavior and the client’s ability to make better choices or cope more effectively. This entails education, modeling, and targeting what Dr. Shapiro calls a future or positive template (2018). It is important for the client to appropriately and properly assimilate the new information gained through the previous prongs (i.e., past, present, and future) by providing them with experiences that ensure future successes.

During recent
Although the standard

The Importance of Past, Present, and Future in EMDR Therapy
The foundation of the three-pronged protocol postulates that earlier memories are processed before current events, and current events are processed before future events. Why is it so important to process these events in this order? What is the effect on the overall treatment result if it is not processed in order of past, present, and future? Earlier life experiences set the groundwork for present events and triggers. Hence, it is useful to reprocess as many of the historical associations with the triggers as possible. Once these associations have been transformed, some, if not many, present triggers will dissipate. There may, however, still be current triggers that exist outside of these channels of association that will need to be targeted and processed independently. Or there may be unprocessed material that surfaces when processing these triggers. These triggers will be the next targets to be processed.
The focus on the future template provides the client an opportunity to imaginally rehearse future circumstances and desired responses. This is yet another opening for unprocessed material to surface. The use of the future template provides the client a means of resolving any anticipatory anxiety that they may still experience in similar future situations. The three-pronged approach appears to be a bottom-up process in that the future is subsumed by the present and the present is subsumed by the past. It has been suggested that bypassing the three-pronged approach as part of the full
TARGETING POSSIBILITIES
TARGETS MAY ARISE IN ANY PART OF THE EMDR THERAPY PROCESS
When a clinician instructs a client to focus on a target in
Throughout Dr. Shapiro’s clinical books (2006, 2018), she refers to several different targets that may arise in certain parts of the process. The past, present, and future targets referred to earlier are the primary focus in the

TYPES OF EMDR TARGETS
As you think about your client sessions, do you recognize any of the types of targets, including the ancillary targets (i.e., other factors that may be contributing to a client’s disturbance) listed in Exhibit 1.5? The following definitions are provided as a refresher:
TARGETS FROM THE PAST
Touchstone Memory
A memory that lays the foundation for a client’s current presenting issue or problem. This is the memory that formed the core of the maladaptive network or dysfunction. It is the first time a client may have believed, “I am not good enough,” or that this conclusion was formed. The touchstone event often, but not necessarily, occurs in childhood or adolescence. Reprocessing will be more spontaneous for the client if the touchstone events can be identified and reprocessed earlier in the treatment.
Example: As an adult, Mary Jane reported being uncomfortable engaging with large groups of people (i.e., 20 or more). She frequently experienced high levels of anxiety before and during office meetings, in church, and at social events. She was nervous, tentative, fearful, and unsure because she could not trust herself to be in control. During the history-taking process, it was discovered that, when she was in the second grade, Mary Jane wet her pants often. She was afraid to use the restroom because she feared its “tall, dark stalls.” Students often teased her, calling her “baby” and yelling out to the other students that she had wet her pants. What she came to believe about herself was, “I cannot trust myself.” This belief carried over into her later life and caused her to react tentatively in group situations.
Primary Events
These are stand-alone events that may emerge during the History-Taking and Treatment Planning, Reprocessing, and Reevaluation Phases, as well as over the course of treatment itself.
Example: Eddie entered therapy months before complaining of headaches and nightmares caused by memories of long-term sexual abuse by his paternal uncle. During treatment, Eddie reported an event involving an automobile accident that occurred 13 years ago. As a result, Eddie still had some anxiousness around driving. This was targeted once the sexual abuse issues had been resolved.
TARGETS FROM THE PRESENT
Circumstances
Situations that stimulate a disturbance.
Example: Having his principal observe one of his classes caused Pierre to flush with anxiety, even though he had been Teacher of the Year three times running and was a 25-year veteran in the public school system as a high school teacher.
Internal or External Triggers
Internal and external cues that can stimulate dysfunctionally stored information and eliciting emotional or behavioral disturbances.
Examples: Sights, sounds, smells, or sensations may be triggers. A client reports becoming triggered by driving on or near a section of roadway where they were involved in a fatal crash in which their best friend was killed. Or a client becomes anxious and ashamed when being questioned by a police officer, even though they have not done anything wrong. The client may react to their own physiological stimuli. For example, they may be triggered by a slightly elevated increase in heart rate, which they fear might lead to a panic attack. One cancer survivor was triggered by an unexplained headache and loss of appetite, leading to fears of recurrence of cancer.
TARGETS FROM THE FUTURE
Future Desired State
How would the client like to be feeling, sensing, believing, perceiving, and behaving today and in the future? What changes would be necessary? The third prong of
Example: Ryan had always been a passive guy who never could say, “No.” “Peace at any cost” was his motto. The touchstone event identified with his conflict-avoidant behavior was a memory of his usually calm mother lunging at his father with a butcher knife during the heat of his father’s verbal attack. Before the night was over, his father had beaten his mother so severely that she was hospitalized for three days. Once this memory had been targeted and reprocessed, Ryan felt more empowered but needed instruction on how to stand up for himself more assertively. After assertiveness training, he was able to imagine himself successfully interacting and responding appropriately in conflict-laden circumstances.
Positive Template (i.e., Imaginal Future Template Development)
A process in which the client uses the adaptive information learned in the previous two prongs to ensure future behavioral success by incorporating patterns of alternative behavioral responses. These patterns require a client to imagine responding differently and positively to real or perceived negative circumstances or situations or significant people.
Example: Joe came home from a business trip and found his wife in bed with his best friend. Joe and his wife had reconciled despite the obvious upheaval it had caused in their already shaky relationship. In the processing of this abrupt discovery, Joe had mostly worked through his reactions and feelings toward his ex-best friend, but he never wanted to interact with him again. However, both worked at the same firm, and it was inevitable that their paths would cross. What the clinician had Joe imagine was a chance meeting with this man and how Joe would like to see this encounter transpire from beginning to end.
OTHER POTENTIAL TARGETS
Node
In terms of the
Example: Jeremy initially entered therapy because he had difficulty interacting professionally with his supervisor. Whenever his boss called or e-mailed asking him to come to his office, Jeremy felt like a small child being summoned to the principal’s office. “What did I do now?” he thought. After a thorough investigation of his past and present, Jeremy related how he felt and reacted around his father. “I always felt as though I had done something wrong.” Jeremy’s father worked and traveled extensively and was not home very much. When he was, Jeremy could find his father in his office working steadily and mostly unaware of the rest of the family activities in their home. His father was gruff and matter of fact and never paid much attention to Jeremy. When he wanted something from Jeremy or would reprimand him for something he did, he would call Jeremy to his office. It was one of those memories that became the target for Jeremy’s presenting issue.
Cluster Memories
These memories form a series of related or similar events and have shared cues, such as an action, person, or location. Each event is representational or generalizable to the other. These nodes are not targeted in the sessions in which they have been identified. The clinician usually keeps an active list of any nodes that arise during reprocessing and reevaluates them later to see if further treatment is necessary.
Example: Anna between the ages of 7 and 10 years was stung by a bee three different times. Each of these events has varying degrees of trauma attached, but each possesses a shared cue, the bees. These are cluster memories and can be grouped together as a single target.
Progression
A progression is a potential node. It generally arises during the reprocessing of an identified target during or between sets (Shapiro, 2018).
Example: Tricia was targeting incidents related to her mother publicly humiliating her when the memory of how her mother acted at her grandfather’s funeral arose. The clinician knew from previous sessions that Tricia had a close, loving relationship with her grandfather and that he was her primary advocate in the family. The clinician wrote down in her notes that her grandfather’s funeral may need to be targeted in and of itself. When a progression (i.e., potential target) arises, it is important not to distract the client from her processing of the current target. Rather, the clinician continues to allow the client to follow the natural processing of the present target and note any disturbance around this event that she may need to explore and target during a future session.
Feeder Memory
This type of memory has been described by Shapiro (2018) as an inaccessible or untapped earlier memory that contributes to a client’s current dysfunction and that subsequently blocks its reprocessing. Unlike progressions, which typically arise spontaneously, feeder memories usually are discovered more by direct inquiry and are touchstone memories that are yet to be identified. If a client becomes stuck during reprocessing, there may be a feeder memory stalling the processing. A feeder memory also differs from a progression in that the feeder memory is an untapped memory related to the current memory being processed. When this type of memory emerges during reprocessing, it should be investigated immediately, especially if a client is blocking on an adolescent or adult memory (Shapiro, 2009–2017a, 2009–2017b). A feeder memory is usually treated before the current memory (i.e.,
Sometimes the identification and spontaneous processing of the feeder memory is sufficient to unblock the processing of the current memory. The feeder memory still needs to be checked following completion of the current memory to determine if it holds any additional disturbance. Sometimes, the current memory needs to be contained and the feeder memory reprocessed (i.e., Phases 3–6) before resuming reprocessing of the current memory.
Example: Brittany was in the midst of reprocessing a disturbing event involving malicious accusations by her mother (i.e., “You’re a slut.” “You must have brought it on somehow.” “You deserved everything that happened.”). These comments were made by her mother after Brittany at the age of 18 years was nearly raped while walking home from school two months earlier. Following several sets of reprocessing and clinical strategies to unblock or shift her processing, Brittany’s level of disturbance did not change. The clinician strategically asked Brittany to focus on the words “I am dirty” (her original negative cognition) and to scan for earlier events in her life that were shameful and humiliating. The memory that finally emerged was the memory of her brothers waving her dirty underwear out a second-story window of their home for all the neighborhood boys to witness. The memory of her brothers’ cruel behavior is what is called a feeder memory.
Blocking Belief
A blocking belief is a belief that stops the processing of an initial target. It is a distorted or irrational conclusion about self, others, or life circumstances (e.g., “It’s not safe to get over this problem.” “If I feel better, I will forget (betray, dishonor, be disloyal) ___________ (fill in the blank).” “I don’t deserve to get over this problem.”). This type of belief may resolve spontaneously during reprocessing or may require being targeted separately. Blocking beliefs typically show themselves when the clinician is evaluating the Subjective Units of Disturbance (
Example: Heather, a sergeant in the military, returned home after sustaining injuries during a rocket attack while on a routine field mission in Afghanistan. Two of her fellow soldiers died from the blast. Heather was hit by flying shrapnel that literally left a hole in her leg. She required two subsequent surgeries, neither of which resulted in removing all the rocket shrapnel from her leg. During recuperation, Heather reported disturbing recurring dreams, flashbacks, and thoughts of the rocket attack, which were frequently accompanied by high levels of anxiety or a panic attack. While reprocessing the event, the sergeant’s negative cognition was “I’m unsafe” and her
Peelback Memory
A peelback memory usually occurs when a touchstone has not been identified and, during reprocessing, other associations begin to “peel back” to expose prior disturbing memories. There is often confusion between a progression and a peelback memory. A peelback memory is an earlier unsuspected memory, whereas a progression is any new associated memory.
Example: After the processing of an earthquake, Taylor continued to exhibit symptoms of
Fears
Fear in the processing of targeted information can become a blocking mechanism. It stalls the process. Dr. Shapiro identified fears to include fear of the clinical outcome of
Example: It is not unusual for a client to express concern or fear that they are not “doing it” (i.e., the process) correctly or is afraid of extreme abreaction or that the clinician cannot handle the potential level of distress that they might express during the reprocessing.
Wellsprings of Disturbance
This phenomenon is indicative of “the presence of a large number of blocked emotions that can be resistant to full
Example: A man who is forced into therapy at the urging of a disgruntled spouse may possess the belief that “real men don’t cry.” This belief may be associated with an earlier traumatic memory and result in the client suppressing any high level of disturbance that might otherwise naturally occur under a current circumstance (e.g., dealing with his wife’s raging episodes). The true level of affective disturbance is never reached by the client, and it is this same level that contributes to the client’s present dysfunction. Earlier experiences taught him that men (or boys) are not allowed to express themselves emotionally. If there is no change in the client’s imagery, body sensations, or insight, but he continues to report a low level of disturbance, the wellspring phenomenon is probably in effect. When present, the clinician may need to provide additional
Blocking Belief = A negative belief about oneself that stalls reprocessing
Wellsprings of Disturbance = Negative Beliefs + Unresolved (Early Memories) + Blocked Emotions
The distinctions between wellsprings of disturbance and blocking beliefs are important because the presence of either determines what course of action a clinician may take to resolve the blocking issues.
Secondary Gain
A secondary gain issue has the potential of keeping a presenting issue from being resolved.
Example: Typical examples involve the following: what would be lost (e.g., a pension check); what need is being satisfied (e.g., special attention); or how current identity is preserved (e.g., “If I get over my pain, I’m abandoning those who have stood by me since the war.” Or, “If I lose my disability, how will I support my family?”).
Channels of Association
Within the targeted memory, events, thoughts, emotions, and physical sensations may spontaneously arise or arise when a client is instructed to go back to target (i.e., return to the original event [incident, experience]). These are called channels of association and may emerge any time during the reprocessing phases (i.e., Phases 3–6).
When cognition based, channels of association may be another level of the same plateau (responsibility/defectiveness or responsibility/action, safety/vulnerability, or power/control [or choice]) or can be another plateau entirely.
Example: Cara was in the middle of reprocessing being robbed (e.g., safety) after a movie one Friday night. After about five or six sets, she remembered that she had failed to zip up her purse while still in the theater when getting her keys out to drive home. She had a huge bank envelope largely visible for anyone to see (i.e., responsibility). When this channel cleared (i.e., continued to remain positive or remained neutral), the clinician took her back to target, and another channel of association emerged. Cara remembered seeing the robber in the movie theater and that he had been intensely staring at her. She decided it was nothing to worry about and went out to her car (e.g., choice, control).
Channels of association may emerge during reprocessing, where related memories, thoughts, images, emotions, and sensations are stored and linked to one another. The following example demonstrates a series of channels related to the client’s emotions.
Example: Cara was robbed after a movie one Friday night. After one set of
Now that you have a clearer picture of what these targets are and how they are related, can you think of examples for each? Recollect targets from some of your reprocessing sessions with clients to help you identify examples of each. Targets—past, present, future—especially ancillary targets, can emerge in any of the three prongs in the
BILATERAL STIMULATION
WHAT DOES IT DO?
When Dr. Shapiro was in the early stages of developing the theory, procedures, and protocol behind
A client’s preferred means of
If the information during reprocessing is not moving or becomes stuck, it is important to have the client agree beforehand on two preferred directions (i.e., back and forth, up and down, or diagonal) or two types of modalities (i.e., eye movements, audio, tapping) from which the client can choose. Thus, if a need for change in direction or modality occurs, the client has agreed to their preferences in advance. Any time a change in

PREFERRED MEANS OF BILATERAL STIMULATION
Shapiro’s (2018) preferred means of
Many studies have focused on investigating the role of eye movements in
Two dominant theories have emerged as a result of these research studies about the effects of eye movement during
Studies suggest that eye movements are superior to tones (van den Hout et al., 2012) and saccadic eye movements are superior on all parameters in all conditions to vertical eye movements (Parker et al., 2008). One study found that eye movements increased the true memory of an event (Parker et al., 2009). No research presently exists to support having the client process with his eyes closed. Lee and Cuijpers (2013) reported positive effects of eye movements in their meta-analysis.
Table 1.12 outlines the randomized studies of hypotheses regarding eye movements in
SHORTER OR LONGER? SLOWER OR FASTER?
During the Preparation Phase,
| 1996 Sharpley, C. F., Montgomery, I. M., & Scalzo, L. (1996). Comparative efficacy of |
| 1997 Andrade, J., Kavanagh, D., & Baddeley, A. (1997). Eye-movements and visual imagery: A working memory approach to the treatment of posttraumatic stress disorder. British Journal of Clinical Psychology, 36, 209–223. https://doi.org/10.1111/j.2044-8260.1997.tb01408.x |
| 2001 Kavanagh, D. J., Freese, S., Andrade, J., & May, J. (2001). Effects of visuospatial tasks on desensitization to emotive memories. British Journal of Clinical Psychology, 40, 267–280. https://doi.org/10.1348/014466501163689 van den Hout, M., Muris, P., Salemink, E., & Kindt, M. (2001). Autobiographical memories become less vivid and emotional after eye movements. British Journal of Clinical Psychology, 40(2), 121–130. https://doi.org/10.1348/014466501163535 |
| 2002 Kuiken, D., Bears, M., Miall, D., & Smith, L. (2002). Eye movement desensitization reprocessing facilitates attentional orienting. Imagination, Cognition and Personality, 21(1), 3–20. https://doi.org/10.2190/L8JX-PGLC-B72R-KD7X |
| 2003 Barrowcliff, A., Gray, N., MacCulloch, S., Freeman, T., & MacCulloch, M. (2003). Horizontal rhythmical eye movements consistently diminish the arousal provoked by auditory stimuli. British Journal of Clinical Psychology, 42(Pt 3), 289–302. https://doi.org/10.1348/01446650360703393 Christman, S. D., Garvey, K. J., Propper, R. E., & Phaneuf, K. A. (2003). Bilateral eye movements enhance the retrieval of episodic memories. Neuropsychology, 17, 221–229. https://doi.org/10.3758/PBR.15.3.515 Saccadic (not tracking) |
| 2004 Barrowcliff, A. L., Gray, N. S., Freeman, T. C. A., & MacCulloch, M. J. (2004). Eye-movements reduce the vividness, emotional valence and electrodermal arousal associated with negative autobiographical memories. Journal of Forensic Psychiatry and Psychology, 15(2), 325–345. https://doi.org/10.1080/14789940410001673042 In testing the reassurance reflex model, |
| 2006 Christman, S. D., Propper, R. E., & Brown, T. J. (2006). Increased interhemispheric interaction is associated with earlier offset of childhood amnesia. Neuropsychology, 20, 336. https://doi.org/10.1037/0894–4105.20.3.336 Servan-Schreiber, D., Schooler, J., Dew, M. A., Carter, C., & Bartone, P. (2006). In this study, patients with single-event |
| 2007 Parker, A., & Dagnall, N. (2007). Effects of bilateral eye movements on gist based false recognition in the DRM paradigm. Brain and Cognition, 63, 221–225. https://doi.org/10.1016/j.bandc.2006.08.005 Bilateral saccadic |
| 2008 Gunter, R. W., & Bodner, G. E. (2008). How eye movements affect unpleasant memories: Support for a working-memory account. Behaviour Research and Therapy, 46(8), 913–931. https://doi.org/10.1016/j.brat.2008.04.006 Support for working-memory account of the benefits of Lee, C. W., & Drummond P. D. (2008). Effects of eye movement versus therapist instructions on the processing of distressing memories. Journal of Anxiety Disorders, 22(5), 801–808. https://doi.org/10.1016/j.janxdis.2007.08.007 Significant reduction in distress for Maxfield, L., Melnyk, W. T., & Hayman, C. A. G. (2008). A working memory explanation for the effects of eye movements in Supported the working memory explanation on the effects of Parker, A., Relph, S., & Dagnall, N. (2008). Effects of bilateral eye movement on retrieval of item, associative and contextual information. Neuropsychology, 22, 136–145. https://doi.org/10.1037/0894-4105.22.1.136 |
| 2008 Bilateral saccadic |
| 2009 Parker, A., Buckley, S., & Dagnall, N. (2009). Reduced misinformation effects following saccadic bilateral eye movements. Brain and Cognition, 69, 89–97. https://doi.org/10.1016/j.bandc.2008.05.009 Supports hypothesis of the effects on episodic memory and interhemispheric activation. |
| 2010 Engelhard, I. M., van den Hout, M. A., Janssen, W. C., & van der Beek, J. (2010a). Eye movements reduce vividness and emotionality of “flashforwards.” Behaviour Research and Therapy, 48, 442–447. https://doi.org/10.1016/j.brat.2010.01.003 In non-dual task condition and while thinking of future-oriented images, Engelhard, I. M., van den Hout, M. A., Janssen, W. C., & van der Beek, J. (2010b). The impact of taxing working memory on negative and positive memories. European Journal of Psychotraumatology, 1, 5623. https://doi.org/10.3402/ejpt.v1i0.5623 Compared Tetris to Kuiken, D., Chudleigh, M., & Racher, D. (2010). Bilateral eye movements, attentional flexibility and metaphor comprehension: The substrate of Found differential effects between |
| 2011 Engelhard, I. M., van den Hout, M. A., Dek, E. C. P., Giele, C. L., van der Wielen, J.-W., Reijnen, M. J., & van Roij, B. (2011). Reducing vividness and emotional intensity of recurrent “flashforwards” by taxing working memory: An analogue study. Journal of Anxiety Disorders, 25, 599–603. https://doi.org/10.1016/j.janxdis.2011.01.009 Found with Samara, Z., Bernet M., Elzinga, B. M., Heleen A., Slagter, H. A., & Nieuwenhuis, S. (2011). Do horizontal saccadic eye movements increase interhemispheric coherence? Investigation of a hypothesized neural mechanism underlying In healthy adults, 30 seconds of bilateral saccadic Schubert, S. J., Lee, C. W., & Drummond, P. D. (2011). The efficacy and psychophysiological correlates of dual-attention tasks in eye movement desensitization and reprocessing ( van den Hout, M. A., Engelhard, I. M., Rijkeboer, M. M., Koekebakker, J., Hornsveld, H., Leer, A., Toffolo, M. B. J., & Akse, N. (2011). |
| 2011 Supports a working memory account of |
| 2012 Smeets, M. A. M., Dijs, M. W., Pervan, I., Engelhard, I. M., & van den Hout, M. A. (2012). Time-course of eye movement-related decrease in vividness and emotionality of unpleasant autobiographical memories. Memory, 20(4), 346–357. https://doi.org/10.1080/09658211.2012.665462 Supports the theory that emotionality reduces only after vividness has dropped. van den Hout, M. A., Rijkeboer, M. T., Engelhard, I. M., Klugkist, I., Hornsveld, H., Toffolo, M., & Cath, D. (2012). Tones inferior to eye movements in the In this study, |
| 2013 de Jongh, A., Ernst, R., Marques, L, & Hornsveld, H. (2013). The impact of eye movements and tones on disturbing memories involving Evidence for the value of employing Nieuwenhuis, S., Elzinga, B. M., Ras, P. H., Berends, F., Duijs, P., Samara, Z., & Slagter, H. A. (2013). Bilateral saccadic eye movements and tactile stimulation, but not auditory stimulation, enhanced memory retrieval. Brain and Cognition, 81, 52–56. https://doi.org/10.1016/j.bandc.2012.10.003 Functional connectivity between the two hemispheres of the brain increased by bilateral activation of the same. |
| 2015 Kearns, M, Engelhard I. M. (2015). Psychophysiological responsivity to script-driven imagery: An exploratory study of the effects of eye movements on public speaking flashforwards. Frontiers in Psychiatry, 6, 115. https://doi.org/10.3389/fpsyt.2015.00115 Using the control condition of imagery and van Veen, S. C., van Schie, K., Wijngaards-de Meij, L. D., Littel, M., Engelhard, I. M., & van den Hout, M. A. (2015). Speed matters: Relationship between speed of eye movements and modification of aversive autobiographical memories. Frontiers in psychiatry, 6(45), 1–9. https://doi.org/10.3389/fpsyt.2015.00045 This study demonstrated that image vividness did not decrease emotionality over time. This is consistent with a working memory hypothesis that states that highly vivid images responded better to fast |
| 2016 Homer, S. R., Deeprose, C., & Andrade, J. (2016). Negative mental imagery in public speaking anxiety: Forming cognitive resistance by taxing visuospatial working memory. Journal of Behavior Therapy and Experimental Psychiatry, 50, 77–82. https://doi.org/10.1016/j.jbtep.2015.05.004 It was established as hypothesized that reduction in vividness of represented imagery (i.e., public speaking was visualized less vividly; generated less anxiety when imagined) was more effected by Sack, M., Zehl, S., Otti, A., Lahmann, C., Henningsen, P., Kruse, J., & Stingl, M. (2016). A comparison of dual attention, eye movements, and exposure only during eye movement desensitization and reprocessing for posttraumatic stress disorder: Results from a randomized clinical trial. Psychotherapy and Psychosomatics, 85(6), 357–365. https://doi.org/10.1159/000447671 When eye fixation and exposure control were compared to bilateral |
Abbreviations:
While using
During the Desensitization Phase, the suggested average number of
Some clients may require shorter or longer and/or slower or faster sets. For instance, clients who are anxious and/or unsure of the process may require longer sets of
| SLOW, SHORT SETS (4–6) Elicit a Relaxation Response (Slows Down the Train) | FAST, LONG SETS (24–36) Elicit an Activation Response (Speeds up the Train) |
|---|---|
| Safe (calm) place Resource development Resource development and installation | Reprocessing Installation Body scan Future template |
In terms of desensitization and speed, eye movements (or passes) that are too slow tend to stimulate a relaxation response and may not facilitate sufficient dual attention. Therefore, it is imperative for optimal processing that the clinician facilitates the passes as fast as the client can comfortably tolerate. In addition, the clinician should avoid long pauses between sets without a specific reason (e.g., the client feels the need for clinician connection). The client is discouraged from talking at any length between sets. It is suggested that the clinician minimally or nonverbally acknowledge what the client has reported and say, “Notice that” or “Go with that.”
Although the purpose of the Installation Phase is to fully integrate a positive self-assessment with the targeted information, there is still the possibility that other associations could emerge that may need to be addressed. The faster, longer sets of
Except for the reprocessing phases of treatment, shorter, slower sets of
Note: If a positive association occurs during reprocessing, do not slow the speed of the
CONTINUOUS BILATERAL STIMULATION
Although there may be clinicians who administer one continuous sequence of
Note: If a clinician uses continuous
| Provides an opportunity for the clinician to determine if processing has occurred based upon the client’s feedback. |
| Gives the client a break from processing, especially if a set contained an intense abreactive response. |
| Helps a client reorient in terms of present time and consequent safety (i.e., helps to keep “one foot in the present”) and thereby facilitates dual awareness. |
| Allows a client to share any new revelations or insights that arise during processing. |
| Allows a clinician to reaffirm a client’s experience throughout the process. |
| Enables a client to better integrate any new information that emerges on a verbal or conscious level. |
| Allows a clinician to continually reassess or judge the need for any additional clinical interventions or strategies. |
| Provides multiple opportunities for a clinician to give and a client to receive encouragement and reassurance. |
| In terms of abreactive responses, it solidifies for a client that they are larger than the disturbing experience and in control as they demonstrate they can approach and distance from the disturbance during these breaks. |
Abbreviation:
Table 1.15 lists what can happen if
| Using long and fast sets when doing stabilization Doing so may activate processing prematurely (i.e., speeds up the train) and cause a client to begin processing any dysfunctionally stored past memories or present triggers. Short, slow sets of |
| Using short and slow sets when doing reprocessing Slow, short |
| Note: Wilson et al. (1996) and Schubert et al. (2011) found that faster |
| Continuing with eye movements if a client reports pain or dryness because of the process If this occurs, switch to a previously agreed upon, alternate form of |
| Pausing too long in between sets There should be a specific reason for pausing too long between sets. Maybe the client is overwhelmed, “needs” to talk, or wants assurance that they are “doing it right.” If the client tends to relay everything that happened between sets, gently explain the information they give is for baseline reasons only (i.e., to let the clinician know where they are in the process), that the “mind is faster than the mouth,” and only minimal information is needed between sets. When a clinician or client talks excessively between sets, it inhibits the reprocessing (i.e., slows the train) of the targeted material. |
| During reprocessing, using sets that are too long or too short Using sets that are too long may cause a client to lose track of the primary event and become overwhelmed with too many thoughts, images, and emotions, and may inhibit or derail processing. Sets that are too short may inhibit processing by not giving a client enough time to initiate complete processing. The rule of thumb is to start with 20-plus sets of eye movements and judge from a client’s response (i.e., facial expression and body language) to determine what the appropriate number of sets is for each individual client. However subtle, a client will usually give a clue as to when a set is complete. |
| Using continuous Using continuous |
| Continuing with It is not uncommon for a client to look at a clinician and say, “Can we take a break right now? I need to say something.” In the event this occurs, simply stop the train and allow the client to unload any material; and restart the train when the client is willing and able. |
Abbreviation:
HOW TO DO EYE MOVEMENTS
Table 1.16 outlines the specific criteria outlined by Shapiro (2018) on the proper and acceptable way to facilitate eye movements in terms of preference, duration, speed, distance, height, and more.
| Before concentrating on emotionally disturbing material Initially using horizontal or diagonal eye movements, find the best fit for a client (e.g., horizontal, vertical, diagonal). Note: The vertical eye movements may be preferred if a client has a history of vertigo. It is also reported to be helpful in reducing extreme emotional nausea, agitation, eye tension, or dizziness. Vertical eye movements have been known to produce a calming effect. Experiment to find a client’s comfort level (i.e., distancing, speed, height). Switch immediately to an alternate form of Generate a full eye movement set by moving a clinician’s hand from one side of a client’s range of vision to the other. The speed of the eye movement should be as rapid as possible and without any undue physical discomfort to a client. Use at least two fingers as a focal point (i.e., two fingers held together is usually the preferred number in American culture). With palm up approximately 12 to 14 inches from a client’s face (i.e., preferably chin to chin or contralateral eyebrow, some say shoulder to shoulder), hold two fingers upright and ask a client, “Is this comfortable?” Note: It is important to determine distance and placement of the eye movement with which a client is the most comfortable prior to the Assessment Phase. Demonstrate the direction of the eye movements by starting in the middle and slowly moving the fingers back and forth in a client’s visual field, and then ending in the center. Evaluate and monitor a client’s ability to track the moving fingers. Start slowly and increase the rate of speed to the fastest a client can comfortably tolerate physically and still keep in their window of emotional intensity. Ask a client during this testing phase if they have any preferences in terms of speed, distance, and height prior to concentrating on any negative emotions or dysfunctional material. |
| After concentrating on emotionally disturbing material Listen to the client’s feedback to determine if adequate processing is taking place at the end of a session. If the client appears comfortable and shifts are occurring, maintain the predetermined speed. If the client is uncomfortable and shifts are not occurring, the clinician may need to adjust the speed, direction, and number of eye movements. If the client appears stuck (i.e., after successive sets of eye movements, the client reports no shifts), change the direction of the eye movement. If a client experiences difficulty (i.e., manifests in irregular eye movements or “bumpiness”) following a clinician’s fingers, attempt to assist the client to establish a more dynamic connection and sense of movement control that results in smoother tracking by instructing the client to “push my fingers with your eyes.” Assess the client’s comfort, preferred speed, and ability to sustain eye movements by listening to their feedback between sets. |
| If the client reports an increase in positive shifts, continue to maintain the same direction, speed, and duration. Note: If a clinician believes it might be beneficial, it is appropriate to experiment. However, a client’s feedback should be the final determinant whether to decrease or increase the duration of a set. Continue If a client experiences weakness in their eye muscles, they may be unable to do more than a few eye movements at a time. If a client is experiencing high levels of anxiety, demonstrates a tracking deficit, or finds them aversive, they may be unable to track hand movements. Note: If this occurs, reprocess the underlying experience of discomfort and, if need be, use the two-handed approach or auditory or tactile stimulation. The two-handed approach entails having the clinician position their closed hands on opposite sides of the client’s visual field at eye level and then alternating raising right and left index fingers while instructing the client to move their eyes from one raised finger to the other. This type of |
Abbreviation:
IS BILATERAL STIMULATION EMDR THERAPY?
IMPORTANT CONCEPTS TO CONSIDER
MEMORY NETWORK ASSOCIATIONS
No one knows what a memory network looks like, but these networks represent the basis of the
STOP SIGNAL
It is important to heed a client’s wishes to ensure a sense of safety in the therapeutic environment.
In the Preparation Phase, the client is asked to provide the clinician with a cue that indicates they want to stop the processing. It may be a hand, finger, or body gesture. The client may simply just turn away or hold their arms up in the air. Whatever the cue is, the processing should be discontinued immediately when used. This allows the client to maintain an ongoing sense of comfort, safety, and control. When this cue to stop is utilized, the clinician assists the client in accessing whatever is needed to stabilize the client and to proceed with the processing. Discontinue all
It is important not to accept words for stop signals (e.g., “Stop,” “No more,” “I can’t do this,” “I want to throw in the towel,” or “Whoa!”) as it may be confused with what is going on in the processing.
The stop signal is tantamount to having a cord on a train the passenger can pull to indicate to the engineer that they want the train to stop for some reason. For instance, the client may need an added rest before the next stop or may want to get off the train. Ultimately, it is the engineer (i.e., clinician) who stops the train when signaled by the client in some way to stop.
At the beginning of each session, the clinician may remind the client of the chosen stop signal by saying, “If at any time you feel you have to stop, raise your hand (i.e., remind client of desired stop signal).”
| “If at any time you feel you have to stop, (remind the client of chosen stop signal).” “Is this a comfortable distance and speed?” |
| Hand gestures |
Hand Signal Time-Out Signal   |
| Body gestures |
| Standing up Crossing arms or knees Putting hands over mouth, ears, or eyes Cyclist stop signal 
|
EMDR Therapy Is Not Hypnosis
A frequent question asked by clients is, “Is
The differences between hypnosis and
WHAT ONCE WAS ADAPTIVE BECOMES MALADAPTIVE
Some behaviors are learned. Some serve us well and others do not. Some serve us for a period in our life and eventually become a nuisance. For example, a client who was repeatedly sexually molested by a relative as a young child may have learned to dissociate during the molestation. This was their automatic coping response to the fear and pain of the trauma at the time of the abuse. Years later, as an adult, they may still find themself dissociating during stressful situations in their work and life. As a child, dissociation was the only response available and allowed them to cope; it worked well at the time. As a maturing adult, the dissociation begins to cause problems at home, at school, and/or at work.
DEVELOPING AND ENHANCING ADAPTIVE NETWORKS OF ASSOCIATION
Before processing of the negative networks may begin, clients with more complex cases may need to access, strengthen, and reinforce positive life experiences and adaptive memories (e.g., positive resources and behaviors, learning, self-esteem). It is possible to access these positive experiences by developing new and enhancing existing positive networks described as follows.
| HYPNOSIS | |
|---|---|
| Integrative psychotherapy model. Efficacious treatment for Bilateral eye movements are utilized. | Medium within which Case reports available that suggest the efficacy of hypnosis for trauma treatment outcomes (Cardena et al., 2009). Bilateral eye movements occur in hypnosis, but usually are ignored (Bramwell, 1906). Theta (Sabourin et al., 1990), beta (De Pascalis & Penna, 2009), or alpha (Meares, 1960) waves are characteristic of hypnotized subjects. |
| During desensitization, the client may be in a state of heightened emotional arousal. | After induction, the client usually is in a deep hypnotic state. |
| Clinician follows a set procedure and generally does not include clinician-generated suggestions (i.e., lacks suggestibility; Hekmat et al., 1994). | There is no set procedure and includes clinician-generated suggestions (i.e., encourage suggestibility). |
| Each set of eye movements lasts about 30 seconds. | Client is in a trance lasting anywhere from 15 to 45 minutes or longer. |
| Memories may emerge, but memory retrieval is not the primary purpose. | Is often used for memory retrieval. |
| Images of memories generally become more distant and less vivid, and more historical. | Images of memories are generally enhanced and made more vivid and experienced in real time. |
| Clients tend to jump from one associative memory to another. | Clients follow a moment-by-moment (“frame by frame”) sequence of events. |
| Eyes are usually open. | Eyes are closed throughout the induction and treatment phase. |
| Uses | Does not use |
| Clients appear more alert, remain conscious, and are less susceptible to inappropriate suggestion. | Clients are less alert, not conscious, and more susceptible to suggestion. |
| Does not induce a trance state. | Induces a trance state. |
| Dual focus of attention is deliberately maintained at all times. | Dual focus of attention may occur (Harford, 2010). |
| For long-term trauma issues, duration of treatment is often brief. | For long-term trauma issues, duration of treatment is often lengthy. |
Abbreviations:
Developing New Positive Networks
(a) New positive experiences are created when the clinician teaches the client safe (calm) place and other stress management and relaxation techniques; (b) the initial introduction of
Enhancing Already Existing Positive Networks
Investigate and determine what positive life experiences and adaptive memories already exist. As the client holds these positive experiences in mind, the clinician implements
Example: Adalia presents with a history of anxiety. The clinician asks the client to imagine a time in her past when she felt empowered and safe and instructs her to imagine how it might have felt to look, feel, and act that way again in a positive way. As she imagines this positive image, the clinician initiates short and slow sets of
Regardless of how and when they come about, it is important for these positive networks to be present and accessible for reprocessing to occur. With clients who have trouble in identifying positive networks of association or role models, plan on a longer preparation time before any processing of negative experiences.
STATE VERSUS TRAIT CHANGE
Shapiro (2008) differentiated between state and trait change. She defined a state change as momentary or transitory, whereas a trait change reflected a permanent change. A state change is a change of mind. It instills a sense of hope in the client. A state change also requires the use of coping mechanisms to continue the change, whereas a trait change no longer requires the same. With a trait change, the client changes how they see or view the event and, as a result, can experience it differently.
When a client changes their perspective about a previous traumatic event and has the needed skills, they can function more appropriately. An example of a state change is the client saying, “I am able to soothe myself by breathing and using my safe (calm) place when my boss asks me to come to his office. I feel much calmer.” A trait change may be, “I am no longer triggered when my boss asks me to come to his office.” To simplify, “states are weather” whereas “traits are climate.” “All traits are states” but “not all states are traits” (Shapiro, 2006). See Table 1.19 for a better understanding of the differences between the two.
| STATE | TRAIT |
|---|---|
| Momentary or transitory change. Change of mind. Coping skills may be required. “I am able to soothe myself by breathing and using my calm/safe place when my boss asks me to come to this office. I feel much calmer.” Resourcing tends to cause state changes. States are weather. | Permanent change. Changes the way a client sees or views an event and thus can experience it differently. Coping skills are not required. “I am no longer triggered when my boss asks me to come to his office.” Processing tends to lead to trait changes. Traits are climate. |
All traits are states, but not all states are traits.
DUAL AWARENESS—INTERNAL/EXTERNAL BALANCE
Dual awareness or mindfulness, or what Dr. Shapiro calls “dual focus of attention” (2018), allows the client to maintain a sense of present awareness and for the client’s internal processes to function without interference during reprocessing. It allows the client to be a nonevaluative observer with respect to whatever emerges during a reprocessing session. It helps the client keep “one foot in the past and one foot in the present.” The client is on the “train” watching the scenery go by.
One of the primary reasons to teach a client grounding and breathing skills and anchoring them in the present is to help them learn to keep one foot in the present while reprocessing something traumatic from their past. This provides them with a dual focus of attention and reduces the possibility or risk of a client dissociating, blanking out, becoming overwhelmed, and/or resisting. Teaching them these skills prior to the reprocessing will help facilitate a smoother therapeutic experience. It also allows the client to maintain a sense of safety in the present while accessing and stimulating negative information from the past. The clinician can solidify the client’s connection to the present by utilizing verbal reassurances, such as “Good,” “You’re doing fine,” “It’s over,” or “You’re safe now.” The clinician may also stop and change the direction or speed of the
ECOLOGICAL VALIDITY (I.E., SOUNDNESS)
In attempting to discern whether a client’s target has been resolved, look at what resolution of this traumatic event would look like in the real world given the individual, the timing, and the situation. To what degree does the current situation “fit” the circumstances? Ask yourself, “If a client was processing a rape that occurred months before and the rapist was still on the loose, would it be appropriate for them to continue to feel fear and demonstrate vigilance around this event?” The answer depends on how their information processing system works. Is there a reason they may be or may think they are still in danger? Is their sense of vigilance and fear around the rapist emotionally appropriate under the circumstances?
How does one recognize ecological validity? And how do you work with it within the
Developed by Joseph Wolpe in 1969, the modified

Abbreviation:
The
If the client still clings to the 1 (or .5 or 2) and “he’s still out there,” you can consider this to be ecologically valid. Ecological validity is one of the reasons the clinician should go directly to the Installation Phase without the client’s
A blocking belief may also arise in the Installation Phase when evaluating the
Dr. Shapiro has been known to say, “Forgiveness is like rain—it may or may not happen.” If a client forgives someone who has hurt them, it does not mean they use poor judgment with respect to that individual (e.g., they will never leave their children with a past abuser). However, clients often arrive at forgiveness or compassion more quickly and more completely than they might with other forms of therapy. A clinician must be alert to not use their own experiences or experiences of their other clients to determine “ecological validity” for any specific client. If processing stops at a certain place, first attempt to remove the block by changing the direction or modality of the
SIDE BENEFITS OF EMDR THERAPY
The primary goal of
Reprocessing will not eliminate any negative thoughts, emotions, or physical sensations that are appropriate to the situation. For example, a client may experience hate toward their abusive, neglectful, and distant mother. In response to ongoing experiences, the client may have developed low levels of self-esteem and confidence. Reprocessing may be successful in improving the client’s self-esteem and other issues, but the client may or may not still feel hatred toward their mother.
HOLISTIC NATURE OF THE APPROACH
Even though it has been around for more than 30 years,
COOKIE-CUTTER APPROACH
USEFUL METAPHORS
TRAIN METAPHOR
While no longer a major form of transportation in America and the experience of riding a train is unfamiliar to many, the use of the train metaphor continues to be Shapiro’s primary means of explaining the intricate principles, protocols, and procedures inherent in
Dr. Shapiro prescribes the use of a train metaphor to help clients move along their processing “tracks.” Reference to and use of this metaphor will be utilized frequently throughout this Primer. During the Desensitization Phase, this metaphor can be applied as a means of noticing yet distancing the client from fear of the trauma. Dr. Shapiro favors this metaphor because it conveys a sense of movement and safety (Shapiro, 2006). The train metaphor may be used throughout the reprocessing as needed. It goes like this: “In order to help you just notice the experience, imagine riding on a train and the feelings, thoughts, etc., are just scenery going by” (Shapiro, 2018).
During the reprocessing, the image of the train going down the track is also used to encourage the client to continue. The passenger is the client, and the scenery represents the dysfunctional information that they are reprocessing. The clinician might say, “It’s just old scenery. Just watch it go by.” This metaphor is a reminder to the client that the train passes the scenery as quickly as it appears.
Dr. Shapiro describes the processing as “metaphorically like moving down a train track” (Shapiro, 2006). From the point of origination to the destination, there are freight depot stops where useless cargo (i.e., dysfunctional information) is unloaded and new, useful cargo (i.e., adaptive information) is loaded (i.e., adaptive resolution). In between stops, resources may need to be loaded for the client to continue the trip down the track, debris may need to be cleared from the track, and/or linkages to adaptive networks can occur. See Exhibit 1.9 for a pictorial rendition of this metaphor. Again, the damaged material is unloaded and discarded at the freight depots found along the track during the stopping and starting of the
Whether suggesting the train or another example, the metaphor is an option being offered to a client if the trauma becomes too much to bear and distancing from it will allow reprocessing to continue. Installation of the metaphor is unnecessary.
During an abreaction, the train metaphor is a useful strategy for supportively assisting a client to allow movement down the tracks. The clinician can assist by saying, “It’s just old information. Watch it like scenery going by.”
Dr. Shapiro also uses the train metaphor to describe information that moves adaptively from dysfunctional to functional. It is a common experience for a client’s once-vivid negative images, affect, and cognitions to become less vivid and less valid while the opposite happens to the positive images, affect, and cognitions. Can you visualize a train traveling down its track? Each time the dysfunctional information is stimulated or when accelerated processing takes place, the train moves down the track and stops. At each stop, the client unloads dysfunctional information and loads more functional or adaptive information. The train continues on this route until it reaches its final destination (i.e., adaptive resolution). One of the important elements of this journey that should not escape the client is that the choice to make a return trip down the same track and revisit the scenery that emerged is optional.


Although seemingly archaic, the use of the train metaphor versus others (i.e., movie theater, river) makes more sense for several reasons. It conveys the sense of movement and safety that Shapiro emphasizes (2018). It is a distancing metaphor. First, the train moves forward at a rapid rate of speed as it distances the client from the trauma while the scenery recedes in the distance at the same rate of speed. In addition, there is a visual barrier between the client who sits on the train and the scenery passing by outside the train. The protective barrier between the client and trauma helps to create a greater sense of safety. See a representation of this idea by the comparison with the other distancing metaphors in Table 1.20.
TUNNEL METAPHOR
Another metaphor used by Shapiro (2018) is driving a car through a tunnel. To get through the tunnel as quickly as possible, the driver will need to increase their pressure on the accelerator (i.e., “You are in a tunnel. Just keep your foot on the pedal and keep moving.”). In
HAND METAPHORS
Using the hand as her prop, Shapiro explained two different aspects of the treatment process by using a metaphor. When she was training clinicians in
With the palm facing outward and fingers pointing downward, Dr. Shapiro would use another hand metaphor to demonstrate the different components of a memory. The top part of the hand represented the memory and the fingers the different aspects of the memory network—sensory (e.g., visual, auditory, olfactory, tactile, gustatory), thoughts, emotions, body sensations, and thoughts and beliefs (see Figure 1.1).
ANCILLARY TARGETS
A yellow or red board in train lingo is a fixed signal to slow and eventually stop a train. When an engineer encounters one of these, they know they need to stop and then, if possible, proceed with caution, depending on what is farther down the line. In some cases, there may be workers and equipment ahead indicating that the track is being repaired, or there may be an obstacle or debris blocking the tracks that needs to be cleared. Blocking beliefs (e.g., “I do not deserve good things” or “If I get over this, I will betray (be disloyal) to my buddies”) and feeder memories (e.g., an unconscious memory that is emotionally feeding the targeted memory network) can activate yellow or red boards. When one of these emerges, it could be an indicator to a clinician that they may need to slow the “train” with successive sets of
SECONDARY GAINS
Secondary-gain issues tend to obstruct or stall processing. Therefore, it is advisable for a clinician to attempt to ferret these out prior to any actual processing taking place. In the History-Taking Phase and Treatment Planning Phase, the clinician may investigate the presence of these gains by asking the client if they are aware of any reasons why processing might be unsuccessful. Is there something a client may be uncomfortable giving up to help resolve the issues they bring to therapy? What other issues are served by the presenting complaint, such as positive consequences (e.g., pension checks); needs (e.g., fear of dishonoring the dead by getting better and moving on; fear of bears may keep a wife from going on camping trips with her husband); or identity issues (e.g., fear of loss of professional or social identity)? Identify what feeds these secondary gains (e.g., low self-esteem, irrational fears, boundary issues, lack of assertiveness). Whatever the issues are, these fears need to be resolved before a successful therapeutic outcome can be expected or maintained. A clinician also needs to ensure that a client has the stability and resources available, which assists them in giving up the gains. Noncompliance may also be related to other fears (e.g., fear of success, fear of terminating therapy, fear of failure). When this occurs, the clinician may ask the client, “What is the worst that could happen?” or “What would change if you were successful?” The secondary-gain issues and fears may need to be addressed before any successful processing can occur.
BLOCKING BELIEFS
Blocking beliefs generally arise during
SUBJECTIVE UNITS OF DISTURBANCE AND THE EMERGENCE OF BLOCKING BELIEFS
If, after repeated applications of different directions and types of
To probe further for a blocking belief, the clinician may ask the client, “Is there a part of you that might have concerns about getting over this problem?” or “What would happen if you were to completely get over this problem?” and initiate one of more sets of
If a dysfunctional blocking belief surfaces and, after successive sets of
VALIDITY OF COGNITION AND THE EMERGENCE OF BLOCKING BELIEFS
Except for the wording, the same procedures cited earlier for blocking beliefs and the
BODY SCAN AND THE EMERGENCE OF BLOCKING BELIEFS
Blocking beliefs can emerge anywhere during
FEEDER MEMORIES
When Shapiro (2018) first began developing and implementing eye movement desensitization (
At this stage of development, Dr. Shapiro also began asking a client to focus on a presently held negative belief and scan back in the past for an earlier time they may have had this negative belief about themself. Because of these changes, Shapiro (2018) wrote, “The theoretical assumption of
The earlier untapped memories that may emerge and appear to continue to feed a client’s current dysfunction and block successful processing are called feeder memories and may arise in any of the three stages of the
There are several ways to elicit the existence of feeder memories from a client: (a) direct questioning, (b) floatback, and (c) affect scan. If a feeder memory surfaces during the processing of another related event, these strategies may be utilized to ascertain the existence of a feeder memory within the reprocessing session or may be targeted later.
In addition to ancillary targets, there are other client obstacles that may obstruct reprocessing. In these cases, the clinician will need to determine the cause and rectify to initiate or continue processing. The obstacles highlighted in Table 1.21 were adapted from Dr. Shapiro’s work (2009–2017a, 2009–2017b).
TO INTERVENE OR NOT TO INTERVENE
As a rule of thumb or when in doubt, do not intervene during reprocessing. Simply say, “Go with that.” There are many indicators of successful processing, such as shifts: (a) in the memory itself; (b) from one memory to another; (c) in the reported changes or the emergence of new images, sounds, cognitive content, levels of affect, or physical sensations; (d) in a client’s self-worth, self-efficacy, affect, and self-assessment; and (e) from dysfunctional to adaptive. It is important for a clinician to remember anything that emerges between sets is related to a client’s experience, and only memories associated in some way with this experience will emerge. To ensure the success of the reprocessing, it is imperative that a client be allowed on his own to discern the importance of the connections of all associations that may arise. As these associations arise and connections are made, the sets are continued, and the need to engage in any complex
| OBSTACLES | REASONS |
|---|---|
| Headaches, nausea, and dizziness | Secondary-gain issues May be artifact of eye movements Client resistance State of hypervigilance May be part of the memory itself May be the result of dissociation or dissociative disorder |
| Client cannot feel | Memory may be processed fully Client cannot tolerate affect Presently held beliefs exist that inhibit feelings (e.g., Big boys don’t cry/If I start to cry, I will never stop. It is dangerous, unsafe, or shameful to express feelings) Cultural or gender restraints or constraints with parents |
| Oververbalizing | May serve as a buffer Client believes he is supposed to talk |
| Client blaming | Client was mandated to therapy (i.e., client uncooperative or unresponsive) Client shuts down experience |
Table 1.22 provides some examples of changes that may occur in multimemory and single-event channels of association. When any of these shifts occur, stay out of the way and say, “Go with that.”
EYE MOVEMENT DESENSITIZATION VERSUS EMDR THERAPY
In 1987, Dr. Shapiro inadvertently discovered the effects of spontaneous eye movements while focusing on disturbing thoughts of her own. She developed standardized procedures and a protocol that she called
While
| CHANGES IN MULTIMEMORY ASSOCIATIVE CHANNELS | EXAMPLES |
|---|---|
| Dominant belief inherent in trauma | The memory of a boat accident brings up an associated memory of being bullied and physically assaulted by classmates in the second grade (both shared the same negative belief, “I am powerless”). |
| Major participant or perpetrator | A client associates being beaten by his mother with his mother driving drunk while he was in the car. |
| Pronounced stimuli | While processing waking up to a bedroom fire set by a lit cigarette, a firefighter remembers an associative memory of being overcome by smoke in a raging prairie fire. |
| Specific type of event | During the processing of a memory when a teller was robbed at gunpoint, an associated memory of being pistol-whipped in a previous robbery years earlier emerges. |
| Dominant physical sensations | As a client processes their childhood memories of being tied to a bedpost by a babysitter while their parents were away, an associated memory of being assaulted and tied up so the perpetrator can flee spontaneously surfaces. |
| Dominant emotions | Disappointment over being passed over for a much-deserved promotion is shared with an associated memory of failing a |
| Images | Change in content or appearance: A father’s outraged face becomes a smiling one. Change to an image of a different but associated event: The image of a father’s outraged face changes to remembering his anger when he failed a class. Change to a different aspect of the same event: The image of a father’s outraged face changes to one of a grief-stricken man. Shift in perspective: A son begins to see the image of his father’s outraged face as more pathetic or laughable. Expansion of a scene to include more details: Original image picture is one where a son sees the outrage on his father’s face upon hearing that his son was expelled from school. As processing continued, the scene opened up; and he suddenly remembered he was expelled because of a physical fight that ensued on school property between his father and himself. The father started the fight. |
| Shifts in the appearance of an image: The image of an outraged father may become larger (or smaller), blurs or fades, becomes closer (or more distant), turns gray or black or white, transforms into a still image, or disappears altogether. | |
| Sounds | Shifts in the sound of a voice: The voice of an outraged father’s voice may become softer, louder, quieter, distorted, or simply becomes mute. Shifts in dialogue: The son suddenly commences to voice words of assertiveness toward his outraged father. Shifts in language: The son is from Germany and reverted to his first language to express his assertiveness toward his outraged father. |
| Cognitions | Emergence of insight: As processing continues, the son suddenly realizes that the outrage his father demonstrates toward him is really about his father’s sense of failure. A polar shift occurs: In the earlier part of processing, the son’s negative cognition (e.g., “I am not good enough”) is replaced by a positive one (e.g., “I am okay as I am”). |
| Emotions | Increases/decreases in intensity: After the first set of Shifts from one emotion to another: The son’s fear of his outraged father changes to disgust, or crying changes to laughter. Shifts toward more appropriate or ecologically valid emotions: The son’s emotion shifts from fear to sadness to disgust during the course of processing. |
| Physical sensations | Reexperiences physical sensations tied to the emotions: The son experiences chest pains and shortness of breath as he processes fear of his father. Experiences physical sensations felt at the time of the original event: The son feels a punch in his stomach as he processed a memory where his outraged father hit him in the gut. Increases/decreases in intensity: The son’s physical sensations of being hit in the stomach become less/more intense during subsequent sets of Shifts in the location: The physical sensation of being hit in the gut moves from the heart to the throat. |
| Shifts in the type of sensations felt in a certain location: The son’s stomach awareness changes from nauseous to tight to feeling empty. |
Abbreviations:
If during
The clinician may find the use of
The
Table 1.23 outlines the differences between
The procedure initially developed by Shapiro (1989a) has evolved to more closely resemble the standard protocol, with deviations as follows (follow the standard Assessment Phase as completely as possible):
ASSESSMENT PHASE
Select a single memory and an image (or picture) that represents the worst part of the memory/incident.
What image (or picture) represents the worst part of the experience?
If no image/picture, When you think of the experience, what do you get?
Identify a negative belief (e.g., “I’m not safe,” “I should have done something,” “I have no control,” or “I am helpless”) which goes best with the target memory or image.
What words go best with the image (or picture) that express your negative belief about yourself now?
Identify a desired
PC , such as “I’m safe now,” “I did the best I could,” or “It’s over.”TABLE 1.23Eye Movement Desensitization VersusEMDR EMD EMDR Informed by desensitization model.
Procedure for desensitization.
Used for decreasing reactions, reducing arousal, and increasing stability to individual memories; symptom reduction while minimizing spontaneous associations to other experiences; and with clients who appear prone to emotional overwhelm, dysregulation, or outside of window of tolerance.Informed by the AIP model.
Psychotherapeutic orientation.
Used for comprehensive cognitive and emotional restructuring.Brief sets of alternating eye movements or tapping facilitate effective desensitization. Longer sets of eye movements, alternating taps and tones, facilitate information reprocessing. Average number of passes is 12–24.
Sets are continued only as long as necessary to desensitize reactions to the target.Average recommended number of passes of BLS is 20–24 to start, lengthen to 36–40 as needed (the number of passes is generally customized to the client’s response).
There is no limit to the number of sets.Treatment effect
Reduction of the fear and anxiety related to the disturbing memory.Comprehensive treatment effect
Reduction in fear and anxiety.
Replacement of negative emotions with positive ones.
Emergence of insight.
Change in body sensations.
Surfacing of new behaviors.
Negative events transformed to adaptive learning experiences.Abbreviations:
AIP , Adaptive Information Processing;BLS , bilateral stimulation;EMD , eye movement desensitization.When you bring up that image (or picture), what would you like (or prefer) to believe about yourself now?
Determine the validity of the client’s
PC (i.e., rate theVoC on a scale of 1–7).When you focus on that image (or picture), how true do those words, (repeat positive cognition), feel to you now on a scale from 1 to 7, where 1 feels completely false and 7 feels completely true?
Identify the associated emotions.
When you bring up that image (or picture) and those words, (repeat negative cognition), what emotion(s) do you feel now?
Determine the level of disturbance (i.e., rate the
SUD on a scale of 0–10) based on the memory or image and the negative belief.From 0, which is neutral or no disturbance, to 10, which is the worst disturbance you can imagine, how disturbing does it feel to you now?
Identify the physical location of the body sensations.
Where do you feel it in your body?
DESENSITIZATION PHASE
8. Instruct the client to focus on the image, the negative belief, and where they feel it in their body, and initiate a set of
BLS (i.e., faster, but with only 12–15 passes; set ofBLS ). Shorter sets ofBLS are utilized withEMD to limit access to associations.I would like you to bring up that image (or picture), those negative words (repeat negative cognition), and notice where you feel it in your body. Just let whatever happens, happen (set of
BLS ).9. After each set of
BLS , instruct the client toTake a breath. (Pause.) Let it go. Then ask, What are you noticing?
The clinician should note the response, and then gently return the client to the target,
NC , and reassess theSUD . After obtaining theSUD , instruct the client to “Just think of that,” and initiate the next set ofBLS (i.e., 12–15).When you bring up that image (or picture) and those negative words, using a scale from 0, which is neutral or no disturbance, to 10, which is the worst disturbance you can imagine, how disturbing does it feel to you now?
10. Repeat this process until the client reports little or no disturbance (i.e.,
SUD = 0 or ecologically sound) and no new intrusive symptoms emerge.11. Once the
SUD has stopped decreasing, the clinician moves to the Installation Phase.When you focus on that image (or picture), do the words, (repeat positive cognition), still fit, or is there another positive statement you feel would be more suitable?
When you focus on that image (or picture), how true do those words, (repeat positive cognition), feel to you now on a scale from 1 to 7, where 1 feels completely false and 7 feels completely true?
Hold the two together. The clinician initiates
BLS .On a scale from 1 to 7, how true do those words, (repeat positive cognition), feel to you now when you focus on the original experience?
The clinician continues to install the
Continue to the Closure phase. See Chapter 6 for a complete transcript using
PRACTICAL TIPS TO REMEMBER
PRACTICE, PRACTICE, PRACTICE
Practice, practice, practice is this Primer’s mantra. In the
FOLLOW THE SCRIPT VERBATIM
Newly trained
If you have been recently trained or have decided to finally put your
The
Consider logging onto the Trauma Recovery/
KNOW YOUR CLIENT
Before you begin using the reprocessing phases, it is important that you know your client well. Know their strengths and weaknesses. Know their abilities and their limitations. Know their ego deficits. Know their coping mechanisms and strategies. Know their support system—or lack of it. Some clients may not be appropriate or ready for
STAY OFF THE TRACKS
The hallmark of
The most appropriate and easiest method to stay out of the way is by consistently maintaining a position of quiet neutrality. During the process, the clinician encourages the client by saying “Good” or “You’re doing fine.” Beyond this, the clinician must be careful not to physically or verbally express what they believe or think about a client’s responses between sets of
TRACKING THE CLIENT
It is important for the clinician to write down as much as possible of what the client says during the Assessment Phase, especially the exact wording of the client’s negative and positive cognitions and key words from their descriptions of traumatic events. Why? Because it is important to use exact wording when activating what the client says. If a client provides a negative cognition, such as “It’s my fault,” and a clinician reframes it as “I’m responsible,” the clinician may have inadvertently distorted what the client originally meant. In doing so, the clinician has also placed themself in the client’s process. Because the clinician reframed it that way, the client may begin to interpret it as “I’m responsible,” simply because the clinician said it. “It’s my fault” and “I am responsible” may or may not mean the same to the client. To the degree that it does not, it can alter the direction of processing. During the remaining reprocessing Phases 4 through 6, clinicians often find it helpful to write down what the client says. However, if writing down what the client says during reprocessing slows, interrupts, or hinders in any way the client’s flow, stop writing and opt to listen and observe more closely what the client is experiencing in the moment.
KEEP IT SIMPLE
In the early days of your
POWER OF NOW
One of the most emphasized words in the
The clinician may need to repeat the “now” over and over to a client. The client may get confused between how they felt “then” about an incident and how they feel “now” and ask questions that indicate their confusion. “Do you mean then or now?” And they could say, “Then it felt awful, but now it does not feel so bad.” If this happens during the Assessment Phase, the clinician may need to reevaluate whether the client has chosen an appropriate target. Remember, the clinician is looking to relieve the client of a memory that is charged with negativity. Use Exhibit 1.10 to help remember this important point.

ONE MORE TIME
A good rule to remember during
When reinforcing a positive effect during the Desensitization, Installation, and Body Scan Phases, the
SOLO RUN
Client selection is always an important part of the
If you are new to
Dr. Shapiro suggests first identifying the “touchstone” event when there may be one (2008). Before proceeding in this direction, however, one must carefully discern whether it is possible for the client to attain successful processing of a touchstone event. This means that the client must be able to tolerate any level of disturbance that may arise. If the touchstone event is chosen for processing and the client becomes too overwhelmed by the experience, much time could be lost by having to “undo” the client’s newly created fear of the process. On the other hand, if you do not target the touchstone event and it arises as a feeder memory, it has the potential to be even more disturbing. The significance of completing a comprehensive history and obtaining informed consent becomes clearer here; that is, it is important for the client to be informed of the potential for accessing feeder memories during the reprocessing of any chosen target.
In this chapter, an attempt has been made to help refamiliarize the reader with basic concepts inherent in
SUMMARY STATEMENTS
EMDR therapy is an integrative psychotherapeutic approach and is guided by theAIP model. TheAIP model “provides the theoretical framework and principles for treatment and an explanation of the basis of pathology and personality development” (Shapiro, 2018). As an integrative psychotherapeutic approach,EMDR therapy is distinct from cognitive behavioral therapy, experiential, and psychodynamic approaches, although it is not exclusive and may be informed by or used together with these approaches.EMDR therapy has eight distinct phases.EMDR therapy is a three-pronged approach addressing the past, the present, and the future.BLS is notEMDR therapy. It is only one component.During the active reprocessing phases of
EMDR therapy, dual awareness should be maintained always: one foot in the present, and one foot in the past.EMDR therapy is a fluid, dynamic approach that entails the clinician using all their clinical skills. It is neither mechanistic nor a cookbook approach.The heart of
EMDR therapy is theAIP model. As such, it is critical that the clinician have a clear understanding of it to proceed withEMDR practice.Practice, practice, practice. This is how we learn the model.
Know your client thoroughly.
Stay out of the client’s way. The reprocessing is about the client, not the clinician.
REFERENCES
- Acierno, R., Tremont, G., Last, C., & Montgomery, D. (1994). Tripartite assessment of the efficacy of eye-movement desensitization in a multiphobic patient. Journal of Anxiety Disorders, 8, 259–276. https://doi.org/10.1016/0887-6185(94)90007-8
- Adler-Tapia, R. (2015). EMDR psychotherapy case conceptualization with a reverse protocol. [Conference presentation]. Twentieth EMDR International Association Conference, Philadelphia, PA.
- Afifi, T. O., Mota, N. P., Dasiewicz, P., MacMillan, H. L., & Sareen, J. (2012). Physical punishment and mental disorders: Results from a nationally representative US sample. Pediatrics, 130(2), 184–192. https://doi.org/10.1542/peds.2011-2947
- Allon, M. (2015). EMDR group therapy with women who were sexually assaulted in the Congo. Journal of EMDR Practice and Research, 9, 28–34. https://doi.org/10.1891/1933-3196.9.1.28
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Author.
- Andrade, J., Kavanagh, D., & Baddeley, A. (1997). Eye-movements and visual imagery: A working memory approach to the treatment of posttraumatic stress disorder. British Journal of Clinical Psychology, 36, 209–223. https://doi.org/10.1111/j.2044-8260.1997.tb01408.x
- Armstrong, M. S., & Vaughan, K. (1996). An orienting response model of eye movement desensitization. Journal of Behavior Therapy & Experimental Psychiatry, 27, 21–32. https://doi.org/10.1016/0005-7916(95)00056-9
- Arseneault, L., Cannon, M., Fisher, H. L., Polanczyk, G., Moffitt, T. E., & Caspi, A. (2011). Childhood trauma and children’s emerging psychotic symptoms: A genetically sensitive longitudinal cohort study. American Journal of Psychiatry, 168, 65–72. https://doi.org/10.1176/appi.ajp.2010.10040567
- Bae, H., Kim, D., & Park, Y. C. (2008). Eye movement desensitization and reprocessing for adolescent depression. Psychiatry Investigation, 5(1), 60–65. https://doi.org/10.4306/pi.2008.5.1.60
- Barrowcliff, A. L., Gray, N. S., Freeman, T. C. A., & MacCulloch, M. J. (2004). Eye-movements reduce the vividness, emotional valence and electrodermal arousal associated with negative autobiographical memories. Journal of Forensic Psychiatry and Psychology, 15(2), 325–345. https://doi.org/10.1080/14789940410001673042
- Barrowcliff, A. L., Gray, N. S., MacCulloch, S., Freeman, T. C., & MacCulloch, M. J. (2003). Horizontal rhythmical eye movements consistently diminish the arousal provoked by auditory stimuli. British Journal of Clinical Psychology, 42(Pt 3), 289–302. https://doi.org/10.1348/01446650360703393
- Behnam Moghadam, M., Alamdari, A. K., Behnam Moghadam, A., & Darban, F. (2015). Effect of EMDR on depression in patients with myocardial infarction. Global Journal of Health Science, 7, 258–262. https://doi.org/10.5539/gjhs.v7n6p258
- Bergmann, U. (2000). Further thoughts on the neurobiology of EMDR: The role of the cerebellum in accelerated information processing. Traumatology, 6(3), 175–200. https://doi.org/10.1177/153476560000600303
- Bergmann, U. (2008). The neurobiology of EMDR: Exploring the thalamus and neural integration. Journal of EMDR Practice and Research, 2(4), 300–314. https://doi.org/10.1891/1933-3196.2.4.300
- Bergmann, U. (2010). EMDR’s neurobiological mechanisms of action: A survey of 20 years of searching. Journal of EMDR Research and Practice, 4, 22–42. https://doi.org/10.1891/1933-3196.4.1.22
- Bisson, J. I., Ehlers, A., Matthews, R., Pilling, S., Richards, D., & Turner, S. (2007). Psychological treatments for chronic posttraumatic stress disorder. Systematic review and meta-analysis. British Journal, 190, 97–104. https://doi.org/10.1192/bjp.bp.106.021402
- Boudewyns, P. A., & Hyer, L. A. (1996). Eye movement desensitization and reprocessing (EMDR) as treatment for posttraumatic stress disorder (PTSD). Clinical Psychology and Psychotherapy, 3, 185–195. https://doi.org/10.1002/(SICI)1099-0879(199609)3:3<185::AID-CPP101>3.0.CO;2-0
- Bramwell, J. M. (1906). Hypnotism. Alexander Moring, Ltd.
- Brown, D. (2006). Treatment of attachment pathology in patients with trauma-related diagnoses. Workshop presented at the Annual Trauma Conference, Harvard Medical School, Boston, MA.
- Brown, K. W., McGoldrick, T., & Buchanan, R. (1997). Body dysmorphic disorder: Seven cases treated with eye movement desensitization and reprocessing. Behavioural and Cognitive Psychotherapy, 25(2), 203–207. https://doi.org/10.1017/S1352465800018403
- Brown, S., & Shapiro, F. (2006). EMDR in the treatment of borderline personality disorder. Clinical Case Studies, 5(5), 403–420. https://doi.org/10.1177/1534650104271773
- Calancie, O. G., Khalid-Khan, S., Booij, L., & Munoz, D. P. (2018). Eye movement desensitization and reprocessing as a treatment for PTSD: Current neurobiological theories and a new hypothesis. Annals of the New York Academy of Science, 1426(1), 127–145. https://doi.org/10.1111/nyas.13882
- Cardena, E., Maldonado, J., van der Hart, O., & Spiegel, D. (2009). Hypnosis. In E. B. Foa, T. M. Keane, & M. J. Friedman (Eds.), Effective treatments for PTSD: Practice guidelines from the International Society for Traumatic Stress Studies (2nd ed., pp. 427–457). Guilford Press.
- Chemtob, C. M., Tolin, D. F., van der Kolk, B. A., & Pitman, R. K. (2000). Eye movement desensitization and reprocessing. In E. B. Foa, T. M. Keane, & M. J. Friedman (Eds.), Effective treatments for PTSD: Practice guidelines from the International Society for Traumatic Stress Studies (pp. 139–155, 333–335). Guilford Press.
- Christman, S. D., Garvey, K. J., Propper, R. E., & Phaneuf, K. A. (2003). Bilateral eye movements enhance the retrieval of episodic memories. Neuropsychology, 17, 221–229. https://doi.org/10.3758/PBR.15.3.515
- Christman, S. D., Propper, R. E., & Brown, T. J. (2006). Increased interhemispheric interaction is associated with earlier offset of childhood amnesia. Neuropsychology, 20, 336. https://doi.org/10.1037/0894–4105.20.3.336
- Davidson, P. R., & Parker, K. C. H. (2001). Eye movement desensitization and reprocessing (EMDR): A meta-analysis. Journal of Consulting and Clinical Psychology, 69, 305–316. https://doi.org/101037//0022–006x.69.2.305
- De Jongh, A., Ernst, R., Marques, L., & Hornsveld, H. (2013). The impact of eye movements and tones on disturbing memories involving PTSD and other mental disorders. Journal of Behavior Therapy and Experimental Psychiatry, 44(4), 477–483. https://doi.org/10.1016/j.jbtep.2013.07.002
- De Pascalis, V., & Penna, P. M. (2009). 40-Hz EEG activity during hypnotic induction and hypnotic testing. International Journal of Clinical and Experimental Hypnosis, 38(2), 125–138. https://doi.org/10.1080/00207149008414507
- de Roos, C., Veenstra, A., de Jongh, A., den Hollander-Gijsman, M., van der Wee, N., Zitman, F., & van Rood, Y. R. (2010). Treatment of chronic phantom limb pain using a trauma-focused psychological approach. Pain Research & Management, 15(2), 65–71. https://doi.org/10.1155/2010/981634
- Devilly, G. J., Spence, S. H., & Rapee, R. M. (1998). Statistical and reliable change with eye movement desensitization and reprocessing: Treating trauma with a veteran population. Behavior Therapy, 29, 435–455. https://doi.org/10.1016/S0005-7894(98)80042-7
- Doering, S., Ohlmeier, M.-C., de Jongh, A., Hofmann, A., & Bisping, V. (2013). Efficacy of a trauma-focused treatment approach for dental phobia: A randomized clinical trial. European Journal of Oral Sciences, 121(6), 584–593. https://doi.org/10.1111/eos.12090
- El Khoury-Malhame, M., Lanteaume, L., Beetz, E. M., Roques, J., Reynaud, E., Samuelian, J. C., Blin, O, Garcia, R., & Khalfa, S. (2011). Attentional bias in post-traumatic stress disorder diminishes after symptom amelioration. Behavior Research and Therapy, 49(11), 796–801. https://doi.org/10.1016/j.brat.2011.08.006
- Elofsson, U. O., von Scheele, B., Theorell, T., & Sondergard, H. P. (2008). Physiological correlates of eye movement desensitization and reprocessing. Journal of Anxiety Disorders, 22(4), 622–634. https://doi.org/10.1016/j.janxdis.2007.05.012
- Engelhard, I. M., van den Hout, M. A., Dek, E. C. P., Giele, C. L., van der Wielen, J.-W., Reijnen, M. J., & van Roij, B. (2011). Reducing vividness and emotional intensity of recurrent “flashforwards” by taxing working memory: An analogue study. Journal of Anxiety Disorders, 25, 599–603. https://doi.org/10.1016/j.janxdis.2011.01.009
- Engelhard, I. M., van den Hout, M. A., Janssen, W. C., & van der Beek, J. (2010a). Eye movements reduce vividness and emotionality of “flashforwards”. Behaviour Research and Therapy, 48, 442–447. https://doi.org/10.1016/j.brat.2010.01.003
- Engelhard, I. M., van den Hout, M. A., Janssen, W. C., & van der Beek, J. (2010b). The impact of taxing working memory on negative and positive memories. European Journal of Psychotraumatology, 1, 5623. https://doi.org/10.3402/ejpt.v1i0.5623
- Faretta, E. (2013). EMDR and cognitive behavioral therapy in the treatment of panic disorder: A comparison. Journal of EMDR Practice and Research, 7, 121–133. https://doi.org/10.1891/1933–3196.7.3.121
- Felitti, V. J., Anda, R. F., Nordenberg, D., Williamson, D. F., Spitz, A. M., Edwards, V., Koss, M. P., & Marks, J. S. (1998). Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The adverse childhood experiences (ACE) study. American Journal of Preventive Medicine, 14, 245–258. https://doi.org/10.1016/S0749-3797(98)00017-8
- Fernandez, I., & Faretta, E. (2007). Eye movement desensitization and reprocessing in the treatment of panic disorder with agoraphobia. Clinical Case Studies, 6(1), 44–63. https://doi.org/10.1177/1534650105277220
- Flannery, R., Jr. (1995). Posttraumatic stress disorder: The victim’s guide to healing & recovery. Crossroad.
- Friedman, D., Goldman, R., Stern, Y., & Brown, T. (2009). The brain’s orienting response: An event-related functional magnetic resonance imaging investigation. Human Brain Mapping, 30(4), 1144–1154. https://doi.org/10.1002/hbm.20587
- Gauhar, M., & Wajid, Y. (2016). The efficacy of EMDR in the treatment of depression. Journal of EMDR Practice and Research, 10(2), 59–69. https://doi.org/10.1891/1933-3196.10.2.59
- Gauvreau, P., & Bouchard, S. (2008). Preliminary evidence for the efficacy of EMDR in treating generalized anxiety disorder. Journal of EMDR Practice and Research, 2(1), 26–40. https://doi.org/10.1891/1933-3196.2.1.26
- Gold, S. D., Marx, B. P., Soler-Baillo, J. M., & Sloan, D. M. (2005). Is life stress more traumatic than traumatic stress? Journal of Anxiety Disorders, 19, 687–698. https://doi.org/10.1016/j.janxdis.2004.06.002.
- Grand, D., & Goldberg, A. (2011). This is your brain on sports: Beating blocks, slumps and performance anxiety for good!. Dog Ear Publishing.
- Gunter, R. W., & Bodner, G. E. (2008). How eye movements affect unpleasant memories: Support for a working-memory account. Behaviour Research and Therapy, 46(8), 913–931. https://doi.org/10.1016/j.brat.2008.04.006
- Harford, P. M. (2010). The integrative use of EMDR and clinical hypnosis in the treatment of adults abused as children. Journal of EMDR Practice and Research, 4(2), 60–75. https://doi.org/10.1891/1933–3196.4.2.60
- Heim, C., Plotsky, P. M., & Nemeroff, C. B. (2004). Importance of studying the contributions of early adverse experience to neurobiological findings in depression. Neuropsychopharmacology, 29, 641–648. https://doi.org/10.1038/sj.npp.1300397
- Heins, M., Simons, C., Lataste, T., Pfeifer, S., Versmissen, D., Lardinois, M., Marcelis, M., Delespaul, P., Krabbendam, L., van Os, J., Myin-Germeys, I. (2011). Childhood trauma and psychosis: A case-control and case-sibling comparison across different levels of genetic liability, psychopathology, and type of trauma. American Journal of Psychiatry, 168, 1286–1294. https://doi.org/10.1176/appi.ajp.2011.10101531.
- Hekmat, H., Groth, S., & Rogers, D. (1994). Pain ameliorating effect of eye movement desensitization. Journal of Behavior Therapy and Experimental Psychiatry, 25(2), 121–129. https://doi.org/10.1016/0005-7916(94)90004-3
- Hofmann, A. (2009). The inverted EMDR standard protocol for unstable complex post-traumatic stress disorder. In M. Luber (Ed.), Eye movement desensitization (EMDR) scripted protocols: Special populations (pp. 313–328). Springer Publishing Company.
- Homer, S. R., Deeprose, C., & Andrade, J. (2016). Negative mental imagery in public speaking anxiety: Forming cognitive resistance by taxing visuospatial working memory. Journal of behavior therapy and experimental psychiatry, 50, 77–82. https://doi.org/10.1016/j.jbtep.2015.05.004
- Hornsveld, H. K., Landwehr, F., Stein, W., Stomp, M. P. H., Smeets, M. A. M., & van den Hout, M. A. (2010). Emotionality of loss-related memories is reduced after recall plus eye movements but not after recall plus music or recall only. Journal of EMDR Practice and Research, 3(4), 106–112. https://doi.org/10.1891/1933–3196.4.3.106
- Kapoula, Z., Yang, Q., Bonnet, A., Bourtoire, P., & Sandretto, J. (2010). EMDR effects on pursuit eye movements. PLoS ONE, 5(5), e10762. https://doi.org/10.1371/journal.pone.0010762
- Kavanagh, D. J., Freese, S., Andrade, J., & May, J. (2001). Effects of visuospatial tasks on desensitization to emotive memories. British Journal of Clinical Psychology, 40, 267–280. https://doi.org/10.1348/014466501163689
- Kearns, M., & Engelhard I. M. (2015). Psychophysiological responsivity to script-driven imagery: An exploratory study of the effects of eye movements on public speaking flashforwards. Frontiers in Psychiatry, 6, 115. https://doi.org/10.3389/fpsyt.2015.00115
- Kip, K. E., Sullivan, K. L., Lengacher, C. A., Rosenzweig, L., Hernandez, D. F., Kadel, R., Kozel, F. A., Shuman, A., Girling, S. A., Hardwick, M. J., & Diamond, D. M. (2013). Brief treatment of co-occurring post-traumatic stress and depressive symptoms by use of accelerated resolution therapy. Frontiers in Psychiatry, 4(11). https://doi.org/10.3389/fpsyt.2013.00011
- Korn, D. L., Maxfield, L., Stickgold, R., & Smyth, N. J. (2018). EMDR Fidelity Rating Scale (EFRS), version 2. https://emdrresearchfoundation.org/research-grants/emdr-fidelity-rating-scale/
- Kristjánsdóttir, K., & Lee, C. W. (2011). A comparison of visual versus auditory concurrent tasks on reducing the distress and vividness of aversive auto-biographical memories. Journal of EMDR Practice and Research, 5(2), 34–41. https://doi.org/10.1891/1933-3196.5.2.34
- Kuiken, D., Bears, M., Miall, D., & Smith, L. (2002). Eye movement desensitization reprocessing facilitates attentional orienting. Imagination, Cognition and Personality, 21(1), 3–20. https://doi.org/10.2190/L8JX-PGLC-B72R-KD7X
- Kuiken, D., Chudleigh, M., & Racher, D. (2010). Bilateral eye movements, attentional flexibility and metaphor comprehension: The substrate of REM dreaming? Dreaming, 20, 227–247. https://doi.org/10.1037/a0020841
- Lee, C. W., & Cuijpers, P. (2013). A meta-analysis of the contribution of eye movements in processing emotional memories. Journal of Behavior Therapy and Experimental Psychiatry, 44(2), 231–239. https://doi.org/10.1016/j.jbtep.2012.11.001
- Lee, C. W., & Drummond, P. D. (2008). Effects of eye movement versus therapist instructions on the processing of distressing memories. Journal of Anxiety Disorders, 22(5), 801–808. https://doi.org/10.1016/j.janxdis.2007.08.007
- Lee, C. W., Taylor, G., & Drummond, P. D. (2006). The active ingredient in EMDR: Is it traditional exposure or dual focus of attention? Clinical Psychology and Psychotherapy, 13(2), 97–107. https://doi.org/10.1002/cpp.479
- Leer, A., Engelhard, I. M., & van den Hout, M. A. (2014). How eye movements in EMDR work: Changes in memory vividness and emotionality. Journal of Behavior Therapy and Experimental Psychiatry, 45(3), 396–401. https://doi.org/10.1016/j.jbtep.2014.04.004
- Lilley, S. A., Andrade, J., Turpin, G., Sabin-Farrell, R., & Holmes, E. A. (2009). Visuospatial working memory interference with recollections of trauma. British Journal of Clinical Psychology, 48, 309–321. https://doi.org/10.1348/014466508X398943
- Lipke, H. (1999). Comments on “thirty years of behavior therapy” and the promise of the application of scientific principles. The Behavior Therapist, 22, 11–14.
- Lohr, J. M., Tolin, D. F., & Kleinknecht, R. A. (1995). An intensive investigation of eye movement desensitization of medical phobias. Journal of Behavior Therapy and Experimental Psychiatry, 26, 141–151. https://doi.org/10.1016/0887-6185(95)00036-4
- Lohr, J. M., Tolin, D. F., & Kleinknecht, R. A. (1996). An intensive investigation of eye movement desensitization of claustrophobia. Journal of Anxiety Disorders, 10, 73–88. https://doi.org/10.1016/0887-6185(95)00036-4
- MacCulloch, M. (2006). Effects of EMDR on previously abused child molesters: Theoretical reviews and preliminary findings from Ricci, Clayton, and Shapiro. Journal of Forensic Psychiatry and Psychology, 17(4), 531–537. https://doi.org/10.1080/14789940601075760
- MacCulloch, M. J., & Feldman, P. (1996). Eye movement desensitisation treatment utilises the positive visceral element of the investigatory reflex to inhibit the memories of post-traumatic stress disorder: A theoretical analysis. British Journal of Psychiatry, 169(5), 571–579. https://doi.org/10.1192/bjp.169.5.571
- Madrid, A., Skolek, S., & Shapiro, F. (2006). Repairing failures in bonding through EMDR. Clinical Case Studies, 5(4), 271–286. https://doi.org/10.1177/1534650104267403
- Maxfield, L., Melnyk, W. T., & Hayman, C. A. G. (2008). A working memory explanation for the effects of eye movements in EMDR. Journal of EMDR Practice and Research, 2(4), 247–261. https://doi.org/10.1891/1933–3196.2.4.247
- McGoldrick, T., Begum, M., & Brown, K. W. (2008). EMDR and olfactory reference syndrome: A case series. Journal of EMDR Practice and Research, 2(1), 63–68. https://doi.org/10.1891/19333196.2.1.63
- Meares, A. (1960). A system of medical hypnosis. The Julian Press.
- Miller, E., & Halpern, S. (1994). Letting go of stress. Inner Peace Music.
- Mol, S. S. L., Arntz, A., Metsemakers, J. F. M., Dinant, G., Vilters-Van Montfort, P. A. P., & Knottnerus, A. (2005). Symptoms of post-traumatic stress disorder after non-traumatic events: Evidence from an open population study. British Journal of Psychiatry, 186, 494–499. https://doi.org/10.1192/bjp.186.6.494
- Nazari, H., Momeni, N., Jariani, M., & Tarrahi, M. J. (2011). Comparison of eye movement desensitization and reprocessing with citalopram in treatment of obsessive-compulsive disorder. International Journal of Psychiatry in Clinical Practice, 15(4), 270–274. https://doi.org/10.3109/13651501.2011.590210
- Nicosia, G. J. (1995). A brief note: Eye movement desensitization and reprocessing is not hypnosis. Dissociation, 8(1), 69.
- Nieuwenhuis, S., Elzinga, B. M., Ras, P. H., Berends, F., Duijs, P., Samara, Z., & Slagter, H. A. (2013). Bilateral saccadic eye movements and tactile stimulation, but not auditory stimulation, enhance memory retrieval. Brain and Cognition, 81, 52–56. https://doi.org/10.1016/j.bandc.2012.10.003
- Obradovic, J., Bush, N. R., Stamperdahl, J., Adler, N. E., & Boyce, W. T. (2010). Biological sensitivity to context: The interactive effects of stress reactivity and family adversity on socioemotional behavior and school readiness. Child Development, 1, 270–289. https://doi.org/10.1111/j.1467–8624.2009.01394.x
- Pace, P. (2003). Connecting ego states through time with EMDR and lifespan integration. [Conference presentation]. Eighth EMDR International Association Conference, Denver, CO.
- Pagani, M., Di Lorenzo, G., Monaco, L., Niolu, C., Siracusano, A., Verardo, A. R., Lauretti, G., Fernandez, I., Nicolais, G., Cogolo, P., & Ammaniti, M. (2011). Pretreatment, intratreatment, and posttreatment EEG imaging of EMDR: Methodology and preliminary results from a single case. Journal of EMDR Practice and Research, 5(2), 42–56. https://doi.org/10.1891/19333196.5.2.42
- Pagani, M., DiLorenzo, G., Verardo, A. R., Nicolais, G., Monaco, L., Lauretti, G., Russo, R., Niolu, C., Ammaniti, M., Fernandex, I., & Siracusano, A. (2012). Neurobiological correlates of EMDR monitoring—an EEG study. PLoS ONE, 7(9), 1–12. https://doi.org/10.1371/journal.pone.0045753
- Parker, A., Buckley, S., & Dagnall, N. (2009). Reduced misinformation effects following saccadic bilateral eye movements. Brain and Cognition, 69, 89–97. https://doi.org/10.1016/j.bandc.2008.05.009
- Parker, A., & Dagnall, N. (2007). Effects of bilateral eye movements on gist based false recognition in the DRM paradigm. Brain and Cognition, 63, 221–225. https://doi.org/10.1016/j.bandc.2006.08.005
- Parker, A., Relph, S., & Dagnall, N. (2008). Effects of bilateral eye movement on retrieval of item, associative and contextual information. Neuropsychology, 22, 136–145. https://doi.org/10.1037/0894–4105.22.1.136
- Patel, G. J., & McDowall, J. (2016). The role of eye movements in EMDR: Conducting eye movements while concentrating on negative autobiographical memories results in fewer intrusions. Journal of EMDR Practice and Research, 10(1), 13–22. https://doi.org/10.1891/1933-3196.10.1.13
- Perkins, B., & Rouanzoin, C. (2002). A critical evaluation of current views regarding eye movement desensitization and reprocessing (EMDR): Clarifying points of confusion. Journal of Clinical Psychology, 58(1), 77–97. https://doi.org/10.1002/jclp.1130
- Pitman, R. K., Orr, S. P., Altman, B., Longpre, R. E., Poire, R. E., & Macklin, M. L. (1996). Emotional processing during eye movement desensitization and reprocessing therapy of Vietnam veterans with chronic posttraumatic stress disorder. Comprehensive Psychiatry, 37, 419–429. https://doi.org/10.1016/S0010–440X(96)90025–5
- Propper, R. E., & Christman, S. D. (2008). Interhemispheric interaction and saccadic horizontal eye movements: Implications for episodic memory, EMDR, and PTSD. Journal of EMDR Practice and Research, 2(4), 269–281. https://doi.org/10.1891/1933-3196.2.4.269.
- Propper, R. E., Pierce, J., Geisler, M. W., Christman, S. D., & Bellorado, N. (2007). Effect of bilateral eye movements on frontal interhemispheric gamma EEG coherence: Implications for EMDR therapy. Journal of Nervous Mental Disorders, 195(9), 785–788. https://doi.org/10.1097/NMD.0b013e318142cf73
- Raboni, M. R., Tufik, S., & Suchecki, D. (2006). Treatment of PTSD by eye movement desensitization reprocessing (EMDR) improves sleep quality, quality of life, and perception of stress. Annals of the New York Academy of Sciences, 1071(1), 508–513. https://doi.org/10.1196/annals.1364.054
- Ray, A. L., & Zbik, A. (2001). Cognitive behavioral therapies and beyond. In C. D. Tollison, J. R. Satterhwaite, & J. W. Tollison (Eds.), Practical pain management (3rd ed., pp. 189–208). Lippincott.
- Read, J., Fosse, R., Moskowitz, A., & Perry, B. (2014). The traumagenic neurodevelopmental model of psychosis revisited. Neuropsychiatry, 4(1), 65–79. https://doi.org/10.2217/NPY.13.89
- Renfrey, G., & Spates, C. R. (1994). Eye movement desensitization: A partial dismantling study. Journal of Behavior Therapy and Experimental Psychiatry, 25, 231–239. https://doi.org/10.1016/0005–7916(94)90023-X
- Ricci, R. J., Clayton, C. A., & Shapiro, F. (2006). Some effects of EMDR on previously abused child molesters: Theoretical reviews and preliminary findings. Journal of Forensic Psychiatry and Psychology, 17(4), 538–562. https://doi.org/10.1080/14789940601070431
- Rimini, D., Molinari, F., Liboni, W., Balbo, M., Daro, R., Viotti, E., & Fernandez, I. (2016). Effect of ocular movements during eye movement desensitization and reprocessing (EMDR) therapy: A near-infrared spectroscopy study. PlusOne, 11(10), e0164379. https://doi.org/10.1371/journal.pone.0164379
- Robinson, J. S., & Larson, C. (2010). Are traumatic events necessary to elicit symptoms of posttraumatic stress? Psychological Trauma: Theory, Research, Practice, and Policy, 2, 71–76. https://doi.org/10.1037/a0018954
- Rogers, S., & Silver, S. M. (2002). Is EMDR an exposure therapy? A review of trauma protocols. Journal of Clinical Psychology, 58(1), 43–59. https://doi.org/10.1002/jclp.1128
- Rogers, S., Silver, S. M., Goss, J., Obenchain, J., Willis, A., & Whitney, R. L. (1999). A single session, group study of exposure and eye movement desensitization and reprocessing in treating posttraumatic stress disorder among Vietnam War veterans: Preliminary data. Journal of Anxiety Disorders, 13(1–2), 119–130. https://doi.org/10.1016/S0887-6185(98)00043-7
- Russell, M. C. (2008). Treating traumatic amputation-related phantom limb pain: A case study utilizing eye movement desensitization and reprocessing within the Armed Services. Clinical Case Studies, 7(2), 136–153. https://doi.org/10.1177/1534650107306292
- Russell, M. C., & Figley, C. R. (2013). Treating traumatic stress injuries in military personnel: An EMDR practitioner’s guide. Routledge Publishing.
- Sabourin, M. E., Cutcomb, S. E., Crawford, H. J., & Pribram, K. (1990). EEG correlates of hypnotic susceptibility and hypnotic trance: Spectral analysis and coherence. International Journal of Psychophysiology, 10, 125–142. https://doi.org/10.1016/0167-8760(90)90027-b
- Sack, M., Hofmann, A., Wizelman, L., & Lempa, W. (2008). Psychophysiological changes during EMDR and treatment outcome. Journal of EMDR Practice and Research, 2(4), 239–246. https://doi.org/10.1891/1933–3196.2.4.239
- Sack, M., Lempa, W., Steinmetz, A., Lamprecht, F., & Hofmann, A. (2008). Alterations in autonomic tone during trauma exposure using eye movement desensitization and reprocessing (EMDR)—Results of a preliminary investigation. Journal of Anxiety Disorders, 22(7), 1264–1271. https://doi.org/10.1016/j.janxdis.2008.01.007
- Sack, M., Zehl, S., Otti, A., Lahmann, C., Henningsen, P., Kruse, J., & Stingl, M. (2016). A comparison of dual attention, eye movements, and exposure only during eye movement desensitization and reprocessing for posttraumatic stress disorder: Results from a randomized clinical trial. Psychotherapy and Psychosomatics, 85(6), 357–365. https://doi.org/10.1159/000447671
- Samara, Z., Bernet, M., Elzinga, B. M., Heleen, A., Slagter, H. A., & Nieuwenhuis, S. (2011). Do horizontal saccadic eye movements increase interhemispheric coherence? Investigation of a hypothesized neural mechanism underlying EMDR. Frontiers in Psychiatry, 2, 4. https://doi.org/10.3389/fpsyt.2011.00004
- Sanderson, A., & Carpenter, R. (1992). Eye movement desensitization versus image confrontation: A single-session crossover study of 58 phobic subjects. Journal of Behavior Therapy and Experimental Psychiatry, 23, 269–275. https://doi.org/10.1016/0005-7916(92)90049-o
- Schneider, J., Hofmann, A., Rost, C., & Shapiro, F. (2007). EMDR and phantom limb pain: Theoretical implications, case study, and treatment guidelines. Journal of EMDR Practice and Research, 1(1), 31–45. https://doi.org/10.1891/1933–3196.1.1.31
- Schneider, J., Hofmann, A., Rost, C., & Shapiro, F. (2008). EMDR in the treatment of chronic phantom limb pain. Pain Medicine, 9(1), 76–82. https://doi.org/10.1111/j.15264637.2007.00299.x
- Schubert, S. J., Lee, C. W., & Drummond, P. D. (2011). The efficacy and psychophysiological correlates of dual-attention tasks in eye movement desensitization and reprocessing (EMDR). Journal of Anxiety Disorders, 25, 1–11. https://doi.org/10.1016/j.janxdis.2010.06.024
- Servan-Schreiber, D., Schooler, J., Dew, M. A., Carter, C., & Bartone, P. (2006). Eye movement desensitization and reprocessing for posttraumatic stress disorder: A pilot blinded, randomized study of stimulation type. Psychotherapy and Psychosomatics, 75(5), 290–297. https://doi.org/10.1159/000093950
- Shapiro, E., & Laub, B. (2014). The recent traumatic episode protocol (R-TEP): An integrative protocol for early EMDR intervention (EEI). In M. Luber (Ed.), Implementing EMDR early mental health interventions for man-made and natural disasters: Models, scripted protocols, and summary sheets (pp. 193–207). Springer Publishing Company.
- Shapiro, F. (1989a). Efficacy of the eye movement desensitization procedure in the treatment of traumatic memories. Journal of Traumatic Stress, 2(2), 199–223. https://doi.org/10.1007/BF00974159
- Shapiro, F. (1989b). Eye movement desensitization: A new treatment for post-traumatic stress disorder. Journal of Behavior Therapy and Experimental Psychiatry, 20(3), 211–217. https://doi.org/10.1016/0005-7916(89)90025-6
- Shapiro, F. (1995). Eye movement desensitization and reprocessing: Basic principles, protocols and procedures (1st ed.). Guilford Press.
- Shapiro, F. (2001). Eye movement desensitization and reprocessing: Basic principles, protocols and procedures (2nd ed.). Guilford Press.
- Shapiro, F. (2002). EMDR as an integrative psychotherapy approach: Experts of diverse orientations explore the paradigm prism. American Psychological Association Press.
- Shapiro, F. (2006). EMDR: New notes on adaptive information processing with case formulations principles, forms, scripts and worksheets, version 1.1. EMDR Institute.
- Shapiro, F. (2007a). EMDR, adaptive information processing, and case conceptualization. Journal of EMDR Practice and Research, 1(2), 68–87. https://doi.org/10.1891/1933-3196.1.2.68
- Shapiro, F. (2007b). EMDR and case conceptualization from an adaptive information processing perspective. In F. Shapiro, F. Kaslow, & L. Maxfield (Eds.), Handbook of EMDR and family therapy processes (pp. 3–36). John Wiley.
- Shapiro, F. (2009–2017a). The EMDR approach to psychotherapy—EMDR Institute basic training course: Weekend 1 of the two part basic training. EMDR Institute.
- Shapiro, F. (2009–2017b). The EMDR approach to psychotherapy—EMDR Institute basic training course: Weekend 2 of the two part basic training. EMDR Institute.
- Shapiro, F. (2012a). EMDR therapy: An overview of current and future research. European Review of Applied Psychology, 62(4), 193–195. https://doi.org/10.1016/j.erap.2012.09.005
- Shapiro, F. (2012b). Getting past your past: Take control of your life with self-help techniques from EMDR therapy. Rodale Books.
- Shapiro, F. (2014). The role of eye movement desensitization and reprocessing (EMDR) therapy in medicine: Addressing the psychological and physical symptoms stemming from adverse life experience. Permanente Journal, 18(1), 71–77. https://doi.org/10.7812/TPP/13–098
- Shapiro, F. (2018). Eye movement desensitization and reprocessing: Basic principles, protocols and procedures (3rd ed.). Guilford Press.
- Shapiro, F., & Forrest, M. S. (2016). EMDR: The breakthrough therapy for overcoming anxiety, stress, and trauma (2nd ed.). Basic Books.
- Shapiro, F., Kaslow, F. W., & Maxfield, M. (2007). Handbook of EMDR and family therapy processes. John Wiley.
- Sharpley, C. F., Montgomery, I. M., & Scalzo, L. (1996). Comparative efficacy of EMDR and alternative procedures in reducing the vividness of mental images. Scandinavian Journal of Behaviour Therapy, 25, 37–42. https://doi.org/10.1080/16506079609456006
- Smeets, M. A. M., Dijs, M. W., Pervan, I., Engelhard, I. M., & van den Hout, M. (2012). Time-course of eye movement-related decrease in vividness and emotionality of unpleasant autobiographical memories. Memory, 20(4), 346–357. https://doi.org/10.1080/09658211.2012.665462
- Solomon, R. M., & Shapiro, F. (2008). EMDR and the adaptive information processing model: Potential mechanisms of change. Journal of EMDR Practice and Research, 2(4), 315–325. https://doi.org/10.1891/1933-3196.2.4.315
- Solomon, S. D., Gerrity, E. T., & Muff, A. M. (1992). Efficacy of treatments for posttraumatic stress disorder: An empirical review. Journal of the American Medical Association, 268, 633–638. https://doi.org/10.1001/jama.1992.03490050081031
- Spates, C. R., Koch, E., Cusack, K., Pagoto, S., & Waller, S. (2009). Eye movement desensitization and reprocessing. In E. B. Foa, T. M. Keane, M. J. Friedman, & J. A. Cohen (Eds.), Effective treatments for PTSD: Practice guidelines from the International Society for Traumatic Stress Studies (2nd ed., pp. 279–305). Guilford Press.
- Stickgold, R. (2002). EMDR: A putative neurobiological mechanism of action. Journal of Clinical Psychology, 58(1), 61–75. https://doi.org/10.1002/jclp.1129
- Stickgold, R. (2008). Sleep-dependent memory processing and EMDR action. Journal of EMDR Practice and Research, 2(4), 289–299. https://doi.org/10.1891/1933-3196.2.4.289
- Suzuki, A., Josselyn, S. A., Frankland, P. W., Masushige, S., Silva, A. J., & Satoshi, K. (2004). Memory reconsolidation and extinction have distinct temporal and biochemical signatures. Journal of Neuroscience, 24(20), 4787–4795. https://doi.org/10.1523/jneurosci.5491-03.2004
- Teicher, M. H., Samson, J. A., Sheu, Y.-S., Polcari, A., & McGreenery, C. E. (2010). Hurtful words: Association of exposure to peer verbal abuse with elevated psychiatric symptom scores and corpus callosum abnormalities. American Journal of Psychiatry, 167, 1464–1471. https://doi.org/10.1176/appi.ajp.2010.10010030
- Uribe, M. E. R., & Ramirez, E. O. L. (2006). The effect of EMDR therapy on the negative information processing on patients who suffer depression. Revista Electrónica de Motivación y Emoción, 9, 23–24.
- van den Berg, D. P. G., & van der Gaag, M. (2012). Treating trauma in psychosis with EMDR: A pilot study. Journal of Behavior Therapy and Experimental Psychiatry, 43(1), 664–671. https://doi.org/10.1016/j.jbtep.2011.09.011
- van den Hout, M. A., Engelhard, I. M., Rijkeboer, M. M., Koekebakker, J., Hornsveld, H., Leer, A., Toffolo, M. B. J., Akse, N. (2011). EMDR: Eye movements superior to beeps in taxing working memory and reducing vividness of recollections. Behaviour Research and Therapy, 49, 92–98. https://doi.org/10.1016/j.brat.2010.11.003
- van den Hout, M. A., & Engelhard, I. (2012). How does EMDR work? Journal of Experimental Psychopathology, 3, 724–738. https://doi.org/10.5127/jep.028212
- van den Hout, M. A., Engelhard, I. M., Smeets, M. A., Hornsveld, H., Hoogeveen, E., and de Heer, E. (2010). Counting during recall: Taxing of working memory and reduced vividness and emotionality of negative memories. Applied Cognitive Psychology, 24(3), 303–311. https://doi.org/10.1002/acp.1677
- van den Hout, M. A., Muris, P., Salemink, E., & Kindt, M. (2001). Autobiographical memories become less vivid and emotional after eye movements. British Journal of Clinical Psychology, 40(2), 121–130. https://doi.org/10.1348/014466501163535
- van den Hout, M. A., Rijkeboer, M. M., Engelhard, I. M., Klugkist, I., Hornsveld, H., Toffolo, M. J., & Cath, D. C. (2012). Tones inferior to eye movements in the EMDR treatment of PTSD. Behaviour Research and Therapy, 50(5), 275–279. https://doi.org/10.1016/j.brat.2012.02.001
- van der Kolk, B. A., Spinazzola, J., Blaustein, M. E., Hopper, J. W., Hopper, E. K., Korn, D. L., & Simpson, W. B. (2007). Randomized clinical trial of eye movement desensitization and reprocessing (EMDR), fluoxetine, and pill placebo in the treatment of posttraumatic stress disorder: Treatment effects and long-term maintenance. Journal of Clinical Psychiatry, 68(1), 37–46. https://doi.org/10.4088/JCP.v68n0105
- van Etten, M. L., & Taylor, S. (1998). Comparative efficacy of treatments for posttraumatic stress disorder: A meta-analysis. Clinical Psychology & Psychotherapy, 5, 126–144. https://doi.org/10.1002/(SICI)1099-0879(199809)
- van Schie, K., Engelhard, I. M., Klugkist, I., & van den Hout, M. A. (2016). Blurring emotional memories using eye movements: Individual differences and speed of eye movements. European Journal of Psychotraumatology, 7, 29476. https://doi.org/10.3402/ejpt.v7.29476
- van Veen, S. C., Engelhard, I. M., & van den Hout, M. A. (2016). The effects of eye movements on emotional memories: using an objective measure of cognitive load. European Journal of Psychotraumatology, 7, 1–11. https://doi.org/10.3402/ejpt.v7.30122
- van Veen, S. C., van Schie, K., Wijngaards-de Meij, L. D., Littel, M., Engelhard, I. M., & van den Hout, M. A. (2015). Speed matters: Relationship between speed of eye movements and modification of aversive autobiographical memories. Frontiers in Psychiatry, 6(45), 1–9. https://doi.org/10.3389/fpsyt.2015.00045
- Varese, F., Smeets, F., Drukker, M., Lieverse, R., Lataster, T., Viechtbauer, W., Read, J., van Os, J., Bentall, R. P. (2012). Childhood adversities increase the risk of psychosis: A meta-analysis of patient-control, prospective- and cross-sectional cohort studies. Schizophrenia Bulletin, 38(4), 661–671. https://doi.org/10.1093/schbul/sbs050
- Wesselmann, D., & Potter, A. E. (2009). Change in adult attachment status following treatment with EMDR: Three case studies. Journal of EMDR Practice and Research, 3(3), 178–191. https://doi.org/10.1891/1933–3196.3.3.178
- Wilensky, M. (2006). Eye movement desensitization and reprocessing (EMDR) as a treatment for phantom limb pain. Journal of Brief Therapy, 5(1), 31–44. https://doi.org/10.1186/1471-2474-14-256
- Wilson, D., Silver, S. M., Covi, W., & Foster, S. (1996). Eye movement desensitization and reprocessing: Effectiveness and autonomic correlates. Journal of Behavior Therapy and Experimental Psychiatry, 27, 219–229. https://doi.org/10.1016/S0005-7916(96)00026-2
- Wolpe, J. (1990). The practice of behavior therapy (4th ed.). Pergamon Press.
- Zarghi, A. (2015). Memory editing with emphasizing the role of EM in EMDR. International Clinical Neuroscience Journal, 2(2), 66–70. https://doi.org/10.22037/icnj.v2i2.9473
